Gamma delta T cell
Gamma delta T cells (γδ T cells) are T cells that have a distinctive T-cell receptor (TCR) on their surface. Most T cells are αβ (alpha beta) T cells with TCR composed of two glycoprotein chains called α (alpha) and β (beta) TCR chains. In contrast, gamma delta (γδ) T cells have a TCR that is made up of one γ (gamma) chain and one δ (delta) chain. This group of T cells is usually much less common than αβ T cells, but are at their highest abundance in the gut mucosa, within a population of lymphocytes known as intraepithelial lymphocytes (IELs).[1]
The antigenic molecules that activate gamma delta T cells are still largely unknown. However, γδ T cells are peculiar in that they do not seem to require antigen processing and major-histocompatibility-complex (MHC) presentation of peptide epitopes, although some recognize MHC class Ib molecules. Furthermore, γδ T cells are believed to have a prominent role in recognition of lipid antigens. They are of an invariant nature and may be triggered by alarm signals, such as heat shock proteins (HSP).
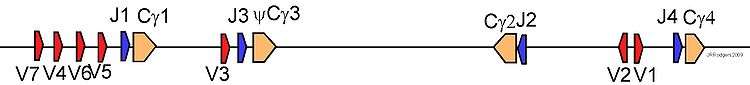
There also exists a γδ-T-cell sub-population within the epidermal compartment of the skin of mice. Originally referred to as Thy-1+ dendritic epidermal cells (Thy1+DEC),[2] these cells are more commonly known as dendritic epidermal T cells (DETC). DETCs arise during fetal development and express an invariant and canonical Vγ3 Vδ1 T-cell receptor [using Garman nomenclature].[3]
Gamma delta T cells in innate and adaptive immunity
The conditions that lead to responses of gamma delta T cells are not fully understood, and current concepts of them as 'first line of defense', 'regulatory cells', or 'bridge between innate and adaptive responses'[1] only address facets of their complex behavior. In fact, gamma delta T cells form an entire lymphocyte system that develops under the influence of other leukocytes, in the thymus and in the periphery. When mature they are divided into functionally distinct subsets that obey their own (mostly unknown) rules and that have countless direct and indirect effects on healthy tissues and immune cells, on pathogens and tissues enduring infections and the host responses to them.
Like other 'unconventional' T cell subsets bearing invariant TCRs, such as CD1d-restricted Natural Killer T cells, gamma delta T cells exhibit several characteristics that place them at the border between the more evolutionarily primitive innate immune system that permits a rapid beneficial response to a variety of foreign agents, and the adaptive immune system, where B and T cells coordinate a slower but highly antigen-specific immune response leading to long-lasting memory against subsequent challenges by the same antigen.
Gamma delta T cells may be considered a component of adaptive immunity in that they rearrange TCR genes to produce junctional diversity and will develop a memory phenotype. However, the various subsets may also be considered part of the innate immunity[4] where a restricted TCR may be used as a pattern recognition receptor.[5] For example, according to this paradigm, large numbers of (human) Vγ9/Vδ2 T cells respond within hours to common molecules produced by microbes, and highly restricted intraepithelial Vδ1 T cells will respond to stressed epithelial cells bearing sentinels of danger.
Recent work has shown that human Vγ9/Vδ2 T cells are also capable of phagocytosis, a function previously exclusive to innate myeloid lineage cells such as neutrophils, monocytes and dendritic cells [6]
Clearly, the complexity of gamma delta T cell biology spans definitions of both innate and adaptive immune responses.
Gene families in different species
Laboratory mice (Mus musculus)
Mouse Vγ chains
This table summarizes the nomenclature of mouse Vγ chains and indicates monoclonal antibodies often used to identify these chains. This system has been best described in strain C57BL/6 and might not apply well to other strains. There are two systems of nomenclature in use (Heilig; Garman), and many writers do not indicate which system they use. For example, the IMGT (International Immunogenetics Information System) uses the Heilig notation, but does not indicate this fact on its website.[7] This table refers to variable chain Vγ gene segments and to monoclonal antibodies that detect the corresponding Vγ protein chains. Note that Adrian Hayday's proposed nomenclature is not widely used, leaving considerable confusion in the literature. One advantage and weakness of the Hayday nomenclature is that it is based on the gene order in the B6 genome, but this might not apply to other strains.
| Heilig and Tonegawa's system[8] |
Garman's system [9] |
"Hayday's system[10]" | antibodies | comments |
|---|---|---|---|---|
| Vγ5 | Vγ3 | GV1S1 | 536; 17D1 specific for Vγ5(Heilig)+Vδ1 clonotype | Skin, Jγ1Cγ1 |
| Vγ6 | Vγ4 | GV2S1 | 17D1; can detect Vγ6Vδ1 when pretreated with GL3 antibodies | reproductive mucosa;Jγ1Cγ1 |
| Vγ4 | Vγ2 | GV3S1 | UC310A6 | lung;Jγ1Cγ1 |
| Vγ7 | Vγ5 | GV4S1 | F2.67 Pereira | most common form in intestinal IEL orthologous to human Vγ1 Jγ1Cγ1 |
| Vγ1 | Vγ1.1 | GV5S1 | 2.11 Pereira 1995 | peripheral lymphoid tissues;Jγ4Cγ4 |
| Vγ2 | Vγ1.2 | GV5S2 | Jγ1Cγ1 | |
| Vγ3 | Vγ1.3 | GV5S3 | Jγ3-pseudoCγ3 |
Human forms
Human Vδ2+ T cells
Vγ9/Vδ2 T cells are unique to humans and primates and represent a minor and unconventional constituent of the leukocyte population in peripheral blood (0.5-5%); yet they are assumed to play an early and essential role in sensing 'danger' by invading pathogens as they expand dramatically in many acute infections and may exceed all other lymphocytes within a few days, e.g. in tuberculosis, salmonellosis, ehrlichiosis, brucellosis, tularemia, listeriosis, toxoplasmosis, and malaria. Of note, all Vγ9/Vδ2 T cells recognize the same small microbial compound (E)-4-hydroxy-3-methyl-but-2-enyl pyrophosphate (HMB-PP), a natural intermediate of the non-mevalonate pathway of isopentenyl pyrophosphate (IPP) biosynthesis.[11] HMB-PP is an essential metabolite in most pathogenic bacteria including Mycobacterium tuberculosis and malaria parasites, but is absent from the human host. Bacterial species that lack the non-mevalonate pathway and synthesize IPP via the classical mevalonate pathway instead, such as Streptococcus, Staphylococcus, and Borrelia, are unable to produce HMB-PP and do not specifically activate Vγ9/Vδ2 T cells.
IPP itself is structurally closely related to HMB-PP and ubiquitously present in all living cells (i.e. also in human cells), yet its potency in vitro is reduced 10,000 fold; whether IPP represents a physiological 'danger' signal of stressed or transformed cells is still unclear. Of pharmacological interest and with bioactivities comparable to that of IPP are synthetic aminobisphosphonates such as zoledronate (Zometa) or pamidronate (Aredia), that are widely used to treat osteoporosis and bone metastases, and incidentally act as Vγ9/Vδ2 T cell receptor agonists. However, increasing evidence suggests that these aminobisphosphonate 'antigens' are not recognised directly by Vγ9/Vδ2 T cells and in fact act indirectly, via their effects on the mevalonate biosynthetic pathway, leading to an accumulation of IPP.[12] Finally, certain alkylated amines have been described to activate Vγ9/Vδ2 T cells in vitro, however only at millimolar concentrations, i.e. with potencies 106-108fold lower than those of HMB-PP, thereby questioning their physiological relevance.
It is still not clear whether these non-peptidic antigens bind directly to the Vγ9/Vδ2 TCR or if a presenting element exists. There is evidence for a requirement for a species-specific cell-cell contact. However, none of the known antigen-presenting molecules like MHC class I and II or CD1 are required for γδ T cell activation suggesting the existence of a novel presenting element. Strong support for a direct recognition of non-peptide antigens by the Vγ9/Vδ2 TCR comes from studies which demonstrated that a transfected Vγ9/Vδ2 TCR can confer responsiveness onto a hitherto unresponsive cell; furthermore, antibodies to the γδ TCR block recognition. Thus, the presence of a functional Vγ9/Vδ2 TCR appears mandatory for a response to non-peptidic antigens although the basis for the huge differences in bioactivity between closely related molecules like HMB-PP and IPP cannot be explained by conventional epitope presentation/recognition models.
These Vγ9Vδ2 T cells can also behave like professional antigen-presenting cells (APC). It seems that human Vγ9Vδ2 T cells are characterized by a specific inflammatory migration program, including multiple receptors for inflammatory chemokines (CXCR3, CCR1, CCR2 and CCR5). It means that the stimulation with IPP or HMB-PP induces migration to the lymphatic tissues, specifically to the T cell area of lymph nodes. So the stimulation of Vγ9Vδ2 T cells with phosphoantigens results in expression of multiple markers which are associated with APC, like MHC I and II molecules, co-stimulatory molecules (CD80, CD86) and adhesion receptors (CD11a, CD18, CD54). Thus activated Vγ9Vδ2 T cells behave like APCs (γδ T-APC) and present antigens to αβ T cells. This leads to turn of naïve CD4+ and CD8+ αβ T cells into effector cells. The differentiation, induced by γδ T-APC, most often led to T helper cell response, in the most of cases to pro-inflammatory Th1 response with subsequent production of IFN-γ and TNF-α. But in the case of a low γδ T-APC: CD4+ ratio it leads to differentiation of some naïve αβ T cells into Th2 (IL-4) or Th0 (IL-4 plus IFN-γ) cells. Human Vγ9Vδ2 T cells are also cells with excellent antigen cross-presentation activity, a process describing the uptake of exogenous antigen and its routing to the MHC I pathway for induction CD8+ cytotoxic T cells. Thus activated cytotoxic T cells can effectively kill infected or tumor cells. This fact can be used in the immunotherapy of cancer and infectious diseases.[13]
Human non-Vδ2+ T cells
The extensive structural diversity of Vδ1 and Vδ3 TCRs and the existence of Vδ1+ clones reactive against MHC, MHC-like, or non-MHC molecules suggest recognition of a highly diverse and heterogeneous set of antigens by non-Vδ2 cells, although cognate interactions between non-Vδ2 TCRs and any of these antigens have not been shown yet. MHC class-I-chain-related gene A (MICA) has also been proposed as an important tumor antigen recognized by Vδ1+ T cells. However, the very low affinity of MICA–Vδ1 TCR interactions estimated by surface plasmon resonance analyses raises doubts about the functional relevance of MICA or MHC class-I-chain-related gene B (MICB) recognition by Vδ1+ TCRs.
Non-Vδ2 γδ T cells are expanded in various infectious contexts involving intracellular bacteria (Mycobacteria and Listeria) as well as extracellular bacteria, such as Borrelia burgdorferi and viruses (HIV, cytomegalovirus). In most instances, the stimuli that trigger Vd1 expansion are not derived from pathogens but instead correspond to endogenous gene products presumably upregulated on infection. The antigens recognized by non-Vδ2 T cells expanded in the above infectious contexts have not been characterized, but the fact that Vδ1+ T-cell responses are not blocked by monoclonal antibody directed against known classical or non-classical MHC molecules suggests recognition of a new class of conserved stress-induced antigens.
See also
- Naive T cells
- Memory T cells
- Helper T cells
- Cytotoxic T cells
- Natural Killer T cells
- Innate immune system
- Adaptive immune system
- Regulatory T cells
References
- 1 2 Holtmeier, W; Kabelitz, D (2005). "Gammadelta T cells link innate and adaptive immune responses". Chemical immunology and allergy. Chemical Immunology and Allergy. 86: 151–83. doi:10.1159/000086659. ISBN 3-8055-7862-8. PMID 15976493.
- ↑ Bergstresser, PR; Sullivan S; Streilein JW; Tigelaar RE. (Jul 1985). "Origin and function of Thy-1+ dendritic epidermal cells in mice". J Invest Dermatol. 85 (1 Suppl): 85s–90s. doi:10.1111/1523-1747.ep12275516. PMID 2409184.
- ↑ Jameson, J; Havran, WL (2007). "Skin gammadelta T-cell functions in homeostasis and wound healing". Immunological reviews. 215: 114–22. doi:10.1111/j.1600-065X.2006.00483.x. PMID 17291283.
- ↑ Born, WK; Reardon, CL; O'Brien, RL (2006). "The function of gammadelta T cells in innate immunity". Current opinion in immunology. 18 (1): 31–8. doi:10.1016/j.coi.2005.11.007. PMID 16337364.
- ↑ Morita, CT; Mariuzza, RA; Brenner, MB (2000). "Antigen recognition by human gamma delta T cells: pattern recognition by the adaptive immune system". Springer seminars in immunopathology. 22 (3): 191–217. doi:10.1007/s002810000042. PMID 11116953.
- ↑ Wu, Y; Wu, W; Wong, WM; Ward, E; Thrasher, AJ; Goldblatt, D; Osman, M; Digard, P; Canaday, DH; Gustafsson, K. (2009). "Human gamma delta T cells: a lymphoid lineage cell capable of professional phagocytosis". Journal of immunology (Baltimore, Md. : 1950). 183 (9): 5622–9. doi:10.4049/jimmunol.0901772. PMID 19843947.
- ↑ IMGT website
- ↑ Heilig, JS; Tonegawa, S (1986). "Diversity of murine gamma genes and expression in fetal and adult T lymphocytes". Nature. 322 (6082): 836–40. doi:10.1038/322836a0. PMID 2943999.
- ↑ Garman, R; Doherty, PJ; Raulet, DH (1986). "Diversity, rearrangement, and expression of murine T cell γ genes". Cell. 45 (5): 733–742. doi:10.1016/0092-8674(86)90787-7. PMID 3486721.
- ↑ Hayday, AC (2000). "gammadelta cells: a right time and a right place for a conserved third way of protection". Annual Review of Immunology. 18: 975–1026. doi:10.1146/annurev.immunol.18.1.975. PMID 10837080.
- ↑ Eberl, M; Hintz, M; Reichenberg, A; Kollas, AK; Wiesner, J; Jomaa, H (2003). "Microbial isoprenoid biosynthesis and human gammadelta T cell activation". FEBS Letters. 544 (1–3): 4–10. doi:10.1016/S0014-5793(03)00483-6. PMID 12782281.
- ↑ Hewitt, RE; Lissina, A; Green, AE; Slay, ES; Price, DA; Sewell, AK (2005). "The bisphosphonate acute phase response: rapid and copious production of proinflammatory cytokines by peripheral blood gd T cells in response to aminobisphosphonates is inhibited by statins". Clinical and experimental immunology. 139 (1): 101–11. doi:10.1111/j.1365-2249.2005.02665.x. PMC 1809263
 . PMID 15606619.
. PMID 15606619. - ↑ Moser, B.; Eberl, M. (Jul 2011). "gammadelta T-APCs: a novel tool for immunotherapy?". Cell Mol Life Sci. 68 (14): 2443–52. doi:10.1007/s00018-011-0706-6.
- Hayday, Adrian C. (2000). "γδ Cells: A Right Time and a Right Place for a Conserved Third Way of Protection". Annual Review of Immunology. 18: 975–1026. doi:10.1146/annurev.immunol.18.1.975. PMID 10837080.
- Girardi, Michael (2006). "Immunosurveillance and Immunoregulation by γδ T Cells". Journal of Investigative Dermatology. 126 (1): 25–31. doi:10.1038/sj.jid.5700003. PMID 16417214.
- Thedrez, A; Sabourin, C; Gertner, J; Devilder, MC; Allain-Maillet, S; Fournié, JJ; Scotet, E; Bonneville, M (2007). "Self/non-self discrimination by human gammadelta T cells: simple solutions for a complex issue?". Immunological reviews. 215: 123–35. doi:10.1111/j.1600-065X.2006.00468.x. PMID 17291284.