Papillary thyroid cancer
| Papillary thyroid cancer | |
|---|---|
|
Papillary thyroid carcinoma. | |
| Classification and external resources | |
| Specialty | oncology |
| ICD-10 | C73 |
| ICD-9-CM | 193 |
| ICD-O | M8260/3 |
| OMIM | 603744 |
| MedlinePlus | 000331 |
| eMedicine | med/2464 |
| MeSH | D013964 |
Papillary thyroid cancer or papillary thyroid carcinoma[1] is the most common type of thyroid cancer,[2] representing 75 percent to 85 percent of all thyroid cancer cases.[1] It occurs more frequently in women and presents in the 20–55 year age group. It is also the predominant cancer type in children with thyroid cancer, and in patients with thyroid cancer who have had previous radiation to the head and neck.[3] It is often well-differentiated, slow-growing, and localized, although it can metastasize.
Diagnosis
Papillary thyroid carcinoma is usually discovered on routine examination as an asymptomatic thyroid nodule that appears as a neck mass. In some instances, the mass may have produced local symptoms. This mass is normally referred to a fine needle aspiration biopsy (FNA) for investigation. FNA accuracy is very high and it is a process widely used in these cases. Other investigation methods include ultrasound imaging and nuclear scan. The ultrasound is a useful test to distinguish solid from cystic lesions and to identify calcifications.[4] The thyroid ultrasound is also very effective to discover microcarcinomas, which refer to very small carcinomas (<1 cm).
Papillary thyroid carcinomas are also discovered when a hard nodule is found in multinodular goiter, when enlarged cervical lymph nodes are detected, or when there are unidentified metastatic lesions elsewhere in the body.[5] Expanding lesions found in the thyroid gland, especially if they are painful, should be examined as they may indicate the presence of papillary thyroid carcinoma. Other clinical signs that could indicate papillary thyroid are: fixation to the trachea, a firm neck mass, damage to recurrent laryngeal or cervical sympathetic nerves. Fifty percent of the population can have thyroid nodules, and the majority will be benign.[6]
Appropriate workup includes an ultrasound of the neck, followed by lab studies. Patients will usually meet with both an endocrinologist and a surgeon (head and neck surgeon or endocrine surgeon).
Markers
Thyroglobulin can be used as a tumor marker for well-differentiated papillary thyroid cancer.[7][8] HBME-1 staining may be useful for differentiating papillary carcinomas from follicular carcinomas; in papillary lesions it tends to be positive.[9]
Reduced expression of ATP5E is significantly associated with the diagnosis of papillary thyroid cancer and may serve as an early tumor marker of the disease.[10]
Pathology
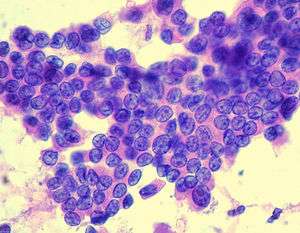
Papillary thyroid cancer gets its name from the papillae among its cells, visible on microscopy. Features include:
- Characteristic Orphan Annie eye nuclear inclusions (nuclei with uniform staining, which appear empty)[11] and psammoma bodies on light microscopy. The former is useful in identifying the follicular variant of papillary thyroid carcinomas.[12]
- Lymphatic spread is more common than hematogenous spread
- Multifocality is common
- The so-called Lateral Aberrant Thyroid is actually a lymph node metastasis from papillary thyroid carcinoma.[13]
- Papillary microcarcinoma is a subset of papillary thyroid cancer defined as measuring less than or equal to 1 cm.[14] The highest incidence of papillary thyroid microcarcinoma in an autopsy series was reported by Harach et al. in 1985, who found 36 of 101 consecutive autopsies to have an incidental microcarcinoma.[15] Michael Pakdaman et al. report the highest incidence in a retrospective surgical series at 49.9 percent of 860 cases.[16] Management strategies for incidental papillary microcarcinoma on ultrasound (and confirmed on FNAB) range from total thyroidectomy with radioactive iodine ablation to observation alone. Harach et al. suggest using the term "occult papillary tumor" to avoid giving patients distress over having cancer. It was Woolner et al. who first arbitrarily coined the term "occult papillary carcinoma" in 1960, to describe papillary carcinomas ≤ 1.5 cm in diameter.[17]
Several variants are recognized, although classical papillary thyroid carcinoma is the most frequent; microscopic, follicular variant, diffuse sclerosing variant, tall cell variant, columnar cell variant, hobnail variant, among others. The encapsulated follicular variant, specifically when noninvasive, has been newly reclassified as the noninvasive follicular thyroid neoplasm with papillary-like nuclear features.[18]
Although papillary carcinoma has a propensity to invade lymphatics, it is less likely to invade blood vessels.[19] These kinds of tumors are most commonly unencapsulated, and they have a high tendency to metastasize locally to lymph nodes, which may produce cystic structures near the thyroid that are difficult to diagnose because of the paucity of malignant tissue.[5][20] Furthermore, papillary tumors may metastasize to the lungs and produce a few nodules or the lung fields may exhibit a snowflake appearance throughout.
Other characteristics of the papillary carcinoma is that E.M. shows increased mitochondria, increased RER, as well as increased apical microvilli. Moreover, papillary carcinomas have an indolent growth, and 40 percent of cases spread out of the capsule.[21]
-
.jpg)
Micrograph of papillary thyroid carcinoma demonstrating prominent papillae with fibrovascular cores. H&E stain.
-
.jpg)
Micrograph showing that the papillae in papillary thyroid carcinoma are composed of cuboidal cells. H&E stain.
-
.jpg)
Micrograph (high power view) showing nuclear changes in papillary thyroid carcinoma (PTC), which include groove formation, optical clearing, eosinophilic inclusions and overlapping of nuclei. H&E stain.
-
.jpg)
Micrograph (high power view) of PTC demonstrating nuclear clearing and overlapping nuclei. H&E stain.
-

Micrograph of metastatic papillary thyroid carcinoma to a lymph node. H&E stain.
-

Micrograph of papillary thyroid carcinoma, tall cell variant - high magnification. H&E stain.
-

Micrograph of papillary thyroid carcinoma, tall cell variant - intermediate magnification. H&E stain.
Associated mutations
Mutations associated with papillary thyroid cancer are mainly two forms of chromosomal translocation and one form of point mutation. These alterations lead to activation of a common carcinogenic pathway—the MAPK/ERK pathway.
Chromosomal translocations involving the RET proto-oncogene (encoding a tyrosine kinase receptor that plays essential roles in the development of neuroendocrine cells) located on chromosome 10q11 occur in approximately a fifth of papillary thyroid cancers. The fusion oncoproteins generated are termed RET/PTC proteins (ret/papillary thyroid carcinoma), and constitutively activate RET and the downstream MAPK/ERK pathway.[1] The frequency of ret/PTC translocations is significantly higher in papillary cancers arising in children and after radiation exposure.[1] The gene NTRK1 (encoding the TrkA receptor), located on chromosome 1q, is similarly translocated in approximately 5 percent to 10 percent of papillary thyroid cancers.[1]
Approximately a third to a half of papillary thyroid carcinomas harbor point mutations in the BRAF oncogene, also activating the MAPK/ERK pathway.[1] In those cases the BRAF mutations found were V600E mutation. After performing a multivariate analysis, it was found that the absence of tumor capsule was the only parameter associated (P=0.0005) with BRAF V600E mutation.[5] According to recent studies, papillary cancers carrying the common V600E mutation tend to have a more aggressive long term course. BRAF mutations are frequent in papillary carcinoma and in undifferentiated cancers that have developed from papillary tumors.
Prognosis
Depending on source, the overall 5-year survival rate for papillary thyroid cancer is 96 percent[22] or 97 percent,[23] with a 10-year survival rate of 93 percent.[22]
For a more specific prognosis for individual cases, there are at minimum 13 known scoring systems for prognosis; among the more often used are:
- AGES - Age, Grade, Extent of disease, Size
- AMES - Age, Metastasis, Extent of disease, Size
- MACIS - Metastasis, Age at presentation, Completeness of surgical resection, Invasion (extrathyroidal), Size[24] (this is a modification of the AGES system). It is probably the most reliable staging method available. Also known as the MAICS system.
- TNM staging - Tumor, node, metastasis. Remarkable about the TNM staging for (differentiated) thyroid carcinoma is that the scoring is different according to age.
MACIS
The MACIS system of estimating the prognosis of papillary thyroid cancer was developed by Clive S. Grant at the Mayo Clinic, and was based on careful evaluation of a large group of patients. It is probably the most reliable staging method available.[25]
It assigns scores to the main factors involved, and uses the sum of this score to calculate the prognosis:
| Factors[25] | Score[25] | |
|---|---|---|
| Distant Metastasis: spread of the cancer to areas outside the neck | Yes | 3 |
| No | 0 | |
| Age at the time the tumor was discovered | Less than 39 years | 3.1 |
| Over 40 years | 0.08 x age | |
| Invasion into surrounding areas of the neck as seen by the naked eye | Yes | 1 |
| No | 0 | |
| Completeness of surgical resection (or removal) of the tumor | Incomplete | 1 |
| Complete | 0 | |
| Size of the tumor | 0.3 x size in cm | |
| Sum of MACIS score[25] | 20 yr Survival[25] |
|---|---|
| < 6.0 | 99% |
| 6.0 - 6.99 | 89% |
| 7.0 - 7.99 | 56% |
| > 8.0 | 24% |
Most patients fall into the low risk category (MACIS score less than 6.0) and are cured of the cancer at the time of surgery.[25]
Children with multiple lung metastases and/or a miliary aspect still have an excellent long-term prognosis if given adequate treatment.[26]
Stage
Based on overall cancer staging into stages I to IV, papillary thyroid cancer has a 5-year survival rate of 100 percent for stages I and II, 93 percent for stage III and 51 percent for stage IV.[27]
Treatment
Surgery remains the mainstay of treatment for papillary thyroid cancer. The Revised 2009 American Thyroid Association guidelines for papillary thyroid cancer state that the initial procedure should be near-total or total thyroidectomy. Thyroid lobectomy alone may be sufficient treatment for small (<1 cm), low-risk, unifocal, intrathyroidal papillary carcinomas in the absence of prior head and neck irradiation or radiologically or clinically involved cervical nodal metastasis.[28]
- Minimal disease (diameter up to 1.0 centimeters) - hemithyroidectomy (or unilateral lobectomy) and isthmectomy may be sufficient. There is some discussion whether this is still preferable over total thyroidectomy for this group of patients.
- Gross disease (diameter over 1.0 centimeters) - total thyroidectomy, and central compartment lymph node removal is the therapy of choice. Additional lateral neck nodes can be removed at the same time if an ultrasound guided FNA and thyrobulin TG cancer washing was positive on the pre-operative neck node ultrasound evaluation.
Arguments for total thyroidectomy are:[29]
- Reduced risk of recurrence, if central compartment nodes are removed at the original surgery.
- 30-85% of papillary carcinoma is multifocal disease. Hemithyroidectomy may leave disease in the other lobe. However, multifocal disease in the remnant lobe may not necessarily become clinically significant or serve as detriment to patient survival.
- Ease of monitoring with thyroglobulin (sensitivity for picking up recurrence is increased in presence of total thyroidectomy, and ablation of remnant normal thyroid by low dose radioiodine 131 after following a low iodine diet (LID).
- Ease of detection of metastatic disease by thyroid and neck node ultrasound.
- Post-operative complications at high-volume thyroid surgery centers with experienced surgeons are comparable to that of hemithyroidectomy.
Arguments for hemithyroidectomy:
- Most patients have low-risk cancer with excellent prognosis, with similar survival outcomes in low-risk patients who undergo total thyroidectomy versus hemithyroidectomy.
- Less likelihood of patient requiring lifelong thyroid hormone replacement after surgery.
Thyroid total body scans are less reliable at finding recurrence than TG and ultrasound.
Papillary tumors tend to be more aggressive in patients over age 45. In such cases it might be required to perform a more extensive resection including portions of the trachea. Also, the sternocleidomastoid muscle, jugular vein, and accessory nerve are to be removed if such procedure allows apparently complete tumor resection. If a significant amount of residual tumor is left in the neck, external radiotherapy has been indicated and has proven useful especially in those cases when residual tumor does not take up radioiodine.
After surgical thyroid removal, the patient waits around 4–6 weeks to then have radioiodine therapy. This therapy is intended to both detect and destroy any metastasis and residual tissue in the thyroid. The treatment may be repeated 6–12 months after initial treatment of metastatic disease where disease recurs or has not fully responded.[30]
Patients are administered hormone replacement levothyroxine for life after surgery, especially after total thyroidectomy. Chemotherapy with cisplatin or doxorubicin has proven limited efficacy, however, it could be helpful for patients with bone metastases to improve their quality of life. Patients are also prescribed levothyroxine and radioiodine after surgery. Levothyroxine influences growth and maturation of tissues and it is involved in normal growth, metabolism, and development. In case of metastases, patients are prescribed antineoplastic agents which inhibit cell growth and proliferation and help in palliating symptoms in progressive disease.
After successful treatment, 35 percent of the patients may experience recurrence within a 40-year span. Also, patients may experience a high incidence of nodule metastasis, with 35 percent cases of cervical node metastases. Approximately 20 percent of patients will develop multiple tumors within the thyroid gland.[31]
There is ongoing discussion regarding the best management regarding the optimal surgical procedure for papillary thyroid cancer. Prognosis of patients with papillary thyroid cancer is found to be dependent on the patient's age, size of the tumor, presence of metastatic disease, and presence of tumor invasion into adjacent tissues near the thyroid gland. Recent studies have examined a more conservative approach to surgery and have demonstrated that hemithyroidectomy may be acceptable for patients with low-risk papillary thyroid cancer with tumor size 1 cm to 4 cm with no presence of invasion to tissues surrounding the thyroid or metastasis. Studies examining large databases of patients with papillary thyroid cancer have concluded that there is no survival advantage for patients with stage I papillary thyroid cancer size 1–4 cm receiving total thyroidectomy versus hemithyroidectomy.[32] In light of this data, choosing the optimal course of surgical and medical management of papillary thyroid cancer should involve shared decision making from patient, endocrinologists, and surgeons.
References
- 1 2 3 4 5 6 Chapter 20 in: Mitchell, Richard Sheppard; Kumar, Vinay; Abbas, Abul K; Fausto, Nelson. Robbins Basic Pathology. Philadelphia: Saunders. ISBN 1-4160-2973-7. 8th edition.
- ↑ Hu MI, Vassilopoulou-Sellin R, Lustig R, Lamont JP "Thyroid and Parathyroid Cancers" in Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ (Eds) Cancer Management: A Multidisciplinary Approach. 11 ed. 2008.
- ↑ Dinets A, Hulchiy M, Sofiadis A, Ghaderi M, Höög A, Larsson C, Zedenius J (2012). "Clinical, Genetic and Immunohistochemical Characterization of 70 Ukrainian Adult Cases with Post-Chornobyl Papillary Thyroid Carcinoma". Eur J Endocrinol. 166: 1049–60. doi:10.1530/EJE-12-0144. PMC 3361791
 . PMID 22457234.
. PMID 22457234. - ↑ "Papillary Thyroid Carcinoma: An Overview". Archives of Pathology & Laboratory Medicine. 2006. Retrieved 2010-07-15.
- 1 2 3 "The Thyroid and its Diseases". Retrieved 2010-07-15.
- ↑ "Papillary Carcinoma Prognosis". Retrieved 2010-07-15.
- ↑ Lin JD (2007). "Thyroglobulin and human thyroid cancer". Clin Chim Acta. 388 (1–2): 15–21. doi:10.1016/j.cca.2007.11.002. PMID 18060877.
- ↑ Tuttle RM, Leboeuf R, Martorella AJ (2007). "Papillary thyroid cancer: monitoring and therapy". Endocrinol. Metab. Clin. North Am. 36 (3): 753–78, vii. doi:10.1016/j.ecl.2007.04.004. PMID 17673127.
- ↑ Papotti M, Rodriguez J, De Pompa R, Bartolazzi A, Rosai J (April 2005). "Galectin-3 and HBME-1 expression in well-differentiated thyroid tumors with follicular architecture of uncertain malignant potential". Mod. Pathol. 18 (4): 541–46. doi:10.1038/modpathol.3800321. PMID 15529186.
- ↑ Hurtado-López, LM; Fernández-Ramírez, F; Martínez-Peñafiel, E; Carrillo Ruiz, JD; Herrera González, NE (16 June 2015). "Molecular Analysis by Gene Expression of Mitochondrial ATPase Subunits in Papillary Thyroid Cancer: Is ATP5E Transcript a Possible Early Tumor Marker?". Medical science monitor : international medical journal of experimental and clinical research. 21: 1745–51. doi:10.12659/MSM.893597. PMID 26079849.
- ↑ "Papillary Carcinoma of Thyroid (Hi Pow)". University of Connecticut Health Center. Retrieved 2008-09-14.
- ↑ Yang GC, Liebeskind D, Messina AV (2001). "Ultrasound-guided fine-needle aspiration of the thyroid assessed by Ultrafast Papanicolaou stain: data from 1135 biopsies with a two- to six-year follow-up". Thyroid. 11 (6): 581–89. doi:10.1089/105072501750302895. PMID 11442006.
- ↑ Escofet X, Khan AZ, Mazarani W, Woods WG (2007). "Lessons to be learned: a case study approach. Lateral aberrant thyroid tissue: is it always malignant?". J R Soc Health. 127 (1): 45–6. doi:10.1177/1466424007073207. PMID 17319317.
- ↑ Shaha AR (2007). "TNM classification of thyroid carcinoma". World J Surg. 31 (5): 879–87. doi:10.1007/s00268-006-0864-0. PMID 17308849.
- ↑ Harach HR, Franssila KO, Wasenius VM (1985). "Occult papillary carcinoma of the thyroid. A "normal" finding in Finland. A systematic autopsy study". Cancer. 56 (3): 531–8. doi:10.1002/1097-0142(19850801)56:3<531::AID-CNCR2820560321>3.0.CO;2-3. PMID 2408737.
- ↑ Pakdaman MN, Rochon L, Gologan O, Tamilia M, Garfield N, Hier MP, Black MJ, Payne RJ (2008). "Incidence and histopathological behavior of papillary microcarcinomas: Study of 429 cases". Otolaryngol Head Neck Surg. 139 (5): 718–22. doi:10.1016/j.otohns.2008.08.014. PMID 18984270.
- ↑ Woolner LB, Lemmon ML, Beahrs OH, Black BM, Keating FR (January 1960). "Occult papillary carcinoma of the thyroid gland: a study of 140 cases observed in a 30-year period". J. Clin. Endocrinol. Metab. 20: 89–105. doi:10.1210/jcem-20-1-89. PMID 13845950.
- ↑ Nikiforov YE, Seethala RR, Tallini G, Baloch ZW, Basolo F, Thompson LDR, Barletta J, Wenig BM, Ghuzlan AA, Kakudo K, Giordano TJ, Alves VA, Khanafshar E, Asa SL, El-Naggar AK, Gooding WE, Hodak SP, Lloyd RV, Maytal G, Mete O, Nikiforova MN, Nosé V, Papotti M, Poller DN, Sadow PM, Tischler AS, Tuttle RM, Wall KB, LiVolsi VA, Randolph GW, Ghossein RA (14 April 2016). "Nomenclature Revision for encapsulated follicular variant of papillary thyroid carcinoma: A Paradigm Shift to Reduce Overtreatment of Indolent Tumors". JAMA Oncol. doi:10.1001/jamaoncol.2016.0386. PMID 27078145.
- ↑ "Thyroid, Papillary Carcinoma". Retrieved 2010-07-15.
- ↑ Grani, G; Fumarola, A (Jun 2014). "Thyroglobulin in Lymph Node Fine-Needle Aspiration Washout: A Systematic Review and Meta-analysis of Diagnostic Accuracy.". The Journal of Clinical Endocrinology and Metabolism. 99 (6): 1970–82. doi:10.1210/jc.2014-1098. PMID 24617715.
- ↑ "Papillary Carcinomas". Archived from the original on April 19, 2010. Retrieved 2010-07-15.
- 1 2 Numbers from National Cancer Database in the US, from Page 10 in: Biersack, H-J; Grünwald, F, eds. (2005). Thyroid Cancer. Berlin: Springer. ISBN 3-540-22309-6. (Note: Book also states that the 14 percent 10-year survival for anaplastic thyroid cancer was overestimated)
- ↑ Rounded up to nearest natural number from 96.7 percent as given by eMedicine > Thyroid, Papillary Carcinoma Author: Luigi Santacroce. Coauthors: Silvia Gagliardi and Andrew Scott Kennedy. Updated: Sep 28, 2010
- ↑ "New York Thyroid Center: Prognosis Staging for Thyroid Cancer". Retrieved 2007-12-22.
- 1 2 3 4 5 6 New York Thyroid Center > Thyroid cancer > Prognosis staging Retrieved on April 30, 2010
- ↑ Vermeer-Mens, J. C. J.; Goemaere, N. N. T.; Kuenen-Boumeester, V.; De Muinck Keizer-Schrama, S. M. P. F.; Zwaan, C. M.; Devos, A. S.; De Krijger, R. R. (2006). "Childhood Papillary Thyroid Carcinoma with Miliary Pulmonary Metastases". Journal of Clinical Oncology. 24 (36): 5788–5789. doi:10.1200/JCO.2006.08.8732. PMID 17179115.
- ↑ cancer.org > Thyroid Cancer By the American Cancer Society. In turn citing: AJCC Cancer Staging Manual (7th ed).
- ↑ Cooper, David (November 2009). "Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer.". Thyroid. 19: 1167–1214. doi:10.1089/thy.2009.0110. PMID 19860577.
- ↑ Udelsman, Robert (July 2005). "Is total thyroidectomy the best possible surgical management for well-differentiated thyroid cancer?". The Lancet Oncology. 6: 529–531. doi:10.1016/s1470-2045(05)70247-3.
- ↑ "Treatment". Retrieved 2010-07-15.
- ↑ "Papillary Thyroid Carcinoma". Archived from the original on July 19, 2008. Retrieved 2010-07-15.
- ↑ Adam, Mohamed (January 2015). "Impact of extent of surgery on survival for papillary thyroid cancer patients younger than 45 years". J Clin Endocrinol Metab.
Endocrine gland
External links
- Thyroidcancer.support www.thyroidcancer.support - thyroid cancer information, support and guidance
- Thyroid cancer at DMOZ
- Cancer Management Handbook: Thyroid and Parathyroid Cancers
- Management Guidelines for Patients with Thyroid Nodules and Differentiated Thyroid Cancer The American Thyroid Association Guidelines Taskforce (2015).
- Thyroid cancer statistics from Cancer Research UK
- International Thyroid Oncology Group (ITOG), a non-profit group devoted to performing clinical trials to advance cures for thyroid cancer.