Triploid syndrome
| Triploid syndrome | |
|---|---|
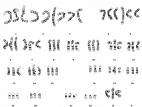 | |
| A karyotype of a person who has this genetic disorder. | |
| Classification and external resources | |
| Specialty | medical genetics |
| ICD-10 | Q92.7 |
| ICD-9-CM | 758.5 |
| DiseasesDB | 32658 |
| MeSH | D057885 |
| Orphanet | 3376 |
Triploid syndrome, also called triploidy, is an extremely rare chromosomal disorder, in which a fetus has three copies of every chromosome instead of the normal two. If this occurs in only some cells, it is called mosaic triploidy, and is less severe.
Signs and symptoms
Many organ systems are affected by triploidy, but the central nervous system and skeleton are the most severely and obviously affected. Common central nervous system defects seen in triploidy include holoprosencephaly, hydrocephalus (water on the brain), ventriculomegaly, Arnold-Chiari malformation, agenesis of the corpus callosum, and neural tube defects. Skeletal manifestations include cleft lip/palate, hypertelorism, club foot, and syndactyly of fingers three and four. Congenital heart defects, hydronephrosis, omphalocele, and meningocele (spina bifida) are also common. Cystic hygromas occur but are uncommon. Triploid fetuses have intrauterine growth restriction beginning early in the pregnancy, as early as 12 weeks, and does not affect the head as severely as the body. Oligohydramnios, low levels of amniotic fluid, is common in triploid pregnancies.[1]
Placental abnormalities are common in triploidy. Most frequently, the placenta is enlarged and may have cysts within. In some cases, the placenta may be unusually small, having ceased to grow.[1]
Diagnosis
Triploidy may be suggested by dramatically elevated levels of serum alpha-fetoprotein. On obstetric ultrasonography, abnormalities of the skeleton, central nervous system, heart, abdomen, and kidneys are visible in the most severe cases beginning at 12-14 weeks of pregnancy. Placental abnormalities associated with a triploid pregnancy become visible at 12-14 weeks. Placentomegaly or intrauterine growth restriction are the typical findings that prompt evaluation for triploidy, though oligohydramnios may be the first sign in some cases. Placentomegaly is not pathognomonic for triploidy because in some cases, the placenta senesces.[1]
Triploidy must be distinguished from trisomy 13 and trisomy 18, which may appear similar on sonography. Genetic testing allows for a definitive diagnosis.[1]
Causes
Triploidy can result from either two sperm fertilizing one egg (60%) or from one sperm fertilizing an egg with two copies of every chromosome (40%).[1]
Prognosis
Most fetuses with triploidy do not survive to birth. Mosaic triploidy has an improved prognosis, but affected individuals have moderate to severe cognitive disabilities. Many people choose to end a triploid pregnancy because full triploidy is incompatible with life.[1]
Epidemiology
Triploidy affects approximately 1-2% of pregnancies, but most miscarry early in development. At birth, males with triploidy are 1.5 times more common than females.[1]
Also known as
- 69,XXX[2]
- 2n/3n Mixoploidy
- 3n Syndrome
- Chromosome Triploidy Syndrome
- Diploid/Triploid Mixoploidy
- Triploidy
- Triploidy Syndrome
See also
References
- 1 2 3 4 5 6 7 Sanders, Roger C. (2002-01-01). Structural Fetal Abnormalities: The Total Picture. Mosby. ISBN 9780323014762.
- ↑ Erol O, Erol M, Karaca M (October 2013). "Complete chorioamniotic separation and persistence of a yolk sac associated with triploidy". Journal of Obstetrics and Gynaecology Canada. 35 (10): 914–6. PMID 24165059.