Universal health coverage by country
Universal health coverage is a broad concept that has been implemented in several ways. The common denominator for all such programs is some form of government action aimed at extending access to health care as widely as possible and setting minimum standards. Most implement universal health care through legislation, regulation and taxation. Legislation and regulation direct what care must be provided, to whom, and on what basis. Usually some costs are borne by the patient at the time of consumption but the bulk of costs come from a combination of compulsory insurance and tax revenues. Some programs are paid for entirely out of tax revenues. In others tax revenues are used either to fund insurance for the very poor or for those needing long term chronic care. The UK government's National Audit Office in 2003 published an international comparison of ten different health care systems in ten developed countries, nine universal systems against one non-universal system (the U.S.), and their relative costs and key health outcomes.[2] A wider international comparison of 16 countries, each with universal health care, was published by the World Health Organization in 2004[3] In some cases, government involvement also includes directly managing the health care system, but many countries use mixed public-private systems to deliver universal health care.
The UN has adopted a resolution on universal health care. It may be the next stage after the Millennium Development Goals.[4]
Africa
Algeria
Algeria operates a public healthcare system. A network of hospitals, clinics, and dispensaries provide treatment to the population, with the Social Security system funding health services, although many people must still cover part of their costs due to the rates paid by the Social Security system unchanged since 1987. The poor are generally entitled to health services free of charge, while the wealthy pay for treatment according to a sliding scale.[5][6]
Botswana
Botswana operates a system of public medical centers, with 98% of health facilities in the country run by the government. All citizens are entitled to be treated in public facilities free of charge, though a nominal fee of $70 is typically charged for public health services except for sexual reproductive health services and antiretroviral therapy services, which are free.[7]
Burkina Faso
Burkina Faso operates a scheme called Universal Health Insurance (AMU) which provides universal healthcare to citizens. It is administered by two separate bodies, one for civilians and the other for the armed forces.[8]
Egypt
Egypt operates a system of public hospitals and clinics through the Ministry of Health. Egyptian citizens can receive treatment at these facilities free of charge. However, those Egyptians who can afford it prefer to pay out of pocket for private healthcare.[9]
Ghana
Ghana operates the National Health Insurance Scheme to provide citizens with health insurance. The level of premiums citizens must pay varies according to their level of income. Most medical facilities are run directly by the Ministry of Health or Ghana Health Service.[10]
Mauritius
The Government of Mauritius operates a system of medical facilities that provide treatment to citizens free of charge.[11]
Morocco
Morocco operates a public health sector run by the government that operates 85% of the country's hospital beds. It deals mainly with the poor and rural populations, who cannot afford private healthcare. In addition, there is a non-profit health sector operated by the National Social Security Fund which covers 16% of the population. There is also a private sector for those who can afford it.[12]
Rwanda
Rwanda operates a system of universal health insurance through the Ministry of Health called Mutuelle de Santé (Mutual Health), a system of community-based insurance where people pay premiums based on their income level into local health insurance funds, with the wealthiest paying the highest premiums and required to cover a small percentage of their medical expenses, while those at the lowest income levels are exempt from paying premiums and can still utilize the services of their local health fund. In 2012, this system insured all but 4% of the population.[13]
South Africa
South Africa has a public healthcare system that provides services to the vast majority of the population, though it is chronically underfunded and understaffed, and a private system that is far better equipped, which covers the wealthier sectors of society.[14]
Tunisia
Tunisia operates a public healthcare system under the National Health Insurance Fund (Caisse Nationale d'Assurance Maladie). All Tunisian citizens and residents can receive treatment in state-run hospitals and clinics free of charge.[15]
Asia
Countries that provide public healthcare in Asia include Bhutan,[16] Bahrain,[17] China, Hong Kong, India, Iran,[18] Israel[19] (see below), Jordan,[20] Kazakhstan,[21] Macau (see below), Malaysia,[22] Mongolia,[23] Oman,[24][25] Singapore, Sri Lanka,[26] Syria,[27] Taiwan (R.O.C.)[28] (see below), Tajikistan,[29] Thailand (see below), Turkey,[30] and Turkmenistan[31] have universal health care.
Bhutan
The Royal Government of Bhutan maintains a policy of free and universal access to primary health care. As hospital facilities in the country are limited, patients with diseases that cannot be treated in Bhutan, such as cancer, are normally referred to hospitals in India for treatment. Such referral treatment is also carried out at the cost of the Royal Government.[32]
Hong Kong
Hong Kong has early health education, professional health services, and well-developed health care and medication system. The life expectancy is 84 for females and 78 for males,[33] which is the second highest in the world, and 2.94 infant mortality rate, the fourth lowest in the world.[34][35]
There are two medical schools in Hong Kong, and several schools offering courses in traditional Chinese medicine. The Hospital Authority is a statutory body that operates and manages all public hospitals. Hong Kong has high standards of medical practice. It has contributed to the development of liver transplantation, being the first in the world to carry out an adult to adult live donor liver transplant in 1993.[36]
India
India's healthcare system is dominated by the private sector, although there are various public healthcare systems like Rajiv Gandhi Jeevandayee Arogya Yojana in Maharashtra that provides free healthcare to those below the poverty line.[37][38] Currently, the majority of Indian citizens do not have health insurance, and must pay out of pocket for treatment. There are government hospitals that provide treatment at taxpayer expense. Some essential drugs are offered free of charge in these hospitals.
An outpatient card at AIIMS costs a one-time fee of 10 rupees (around 20 cents U.S.) and thereafter outpatient medical advice is free. In-hospital treatment costs depend on the financial condition of the patient and the facilities utilized, but are usually much less than the private sector. For instance, a patient is waived treatment costs if their income is below the poverty line. However, getting treatment at high quality government hospitals is very tough due to the high number of people needing healthcare and the lack of sufficient facilities.
Primary health care is provided by city and district hospitals and rural primary health centres (PHCs). These hospitals provide treatment free of cost, but only if they are functional. Primary care is focused on immunization, prevention of malnutrition, pregnancy, child birth, postnatal care, and treatment of common illnesses. Patients who receive specialized care or have complicated illnesses are referred to secondary (often located in district and taluk headquarters) and tertiary care hospitals (located in district and state headquarters or those that are teaching hospitals).
Now organizations like Hindustan Latex Family Planning Promotional Trust and other private organizations have started creating hospitals and clinics in India, which also provide free or subsidized health care and subsidized insurance plans.
The government-run healthcare suffers from a lack of hygiene; the rich avoid the government hospitals and go to private hospitals. With the advent of privatized healthcare, this situation has changed. India now has medical tourism for people from other countries while its own poor find high-quality healthcare either inaccessible or unaffordable.
The current Indian government is planning to unveil a national universal healthcare system called the National Health Assurance Mission, which will provide all Indian citizens with insurance coverage for serious illnesses, and free drugs and diagnostic treatments.[39]
Israel

Israel has a system of universal healthcare as set out by the 1995 National Health Insurance Law. The state is responsible for providing health services to all residents of the country, who can register with one of the four national health service funds. To be eligible, a citizen must pay a health insurance tax. Coverage includes medical diagnosis and treatment, preventive medicine, hospitalization (general, maternity, psychiatric and chronic), surgery and transplants, preventive dental care for children, first aid and transportation to a hospital or clinic, medical services at the workplace, treatment for drug abuse and alcoholism, medical equipment and appliances, obstetrics and fertility treatment, medication, treatment of chronic diseases and paramedical services such as physiotherapy and occupational therapy.[40]
In Israel, the National Health Insurance Law (or National Health Insurance Act) is the legal framework which enables and facilitates basic, compulsory universal health care. The Law was put into effect by the Knesset on January 1, 1995, and was based on recommendations put forward by a National Committee of Inquiry headed by Shoshana Netanyahu which examined restructuring the health care system in Israel in the late 1980s. Prior to the law's passage over 90% of the population was already covered by voluntarily belonging to one of four nationwide, not-for-profit sickness funds which operated some of their own medical facilities and were funded in part by employers and the government and in part by the insured by levies which varied according to income. However, there were three problems associated with this arrangement. First, membership in the largest fund, Clalit, required one to belong to the Histadrut labor organization, even if a person did not wish to (or could not) have such an affiliation while other funds restricted entry to new members based on age, pre-existing conditions or other factors. Second, different funds provided different levels of benefit coverage or services to their members and lastly was the issue mentioned above whereby a certain percentage of the population, albeit a small one, did not have health insurance coverage at all.
Before the law went into effect, all the funds collected premiums directly from members. However, upon passage of the law, a new progressive national health insurance tax was levied through Israel's social security agency which then re-distributes the proceeds to the sickness funds based on their membership and its demographic makeup. This ensured that all citizens would now have health coverage. While membership in one of the funds now became compulsory for all, free choice was introduced into movement of members between funds (a change is allowed once every six months), effectively making the various sickness funds compete equally for members among the populace. Annually, a committee appointed by the ministry of health publishes a "basket" or uniform package of medical services and prescription formulary which all funds must provide as a minimum service to all their members. Achieving this level of equality ensured that all citizens are guaranteed to receive basic healthcare regardless of their fund affiliation which was one of the principal aims of the law. An appeals process was put in place to handle rejection of treatments and procedures by the funds and evaluating cases falling outside the "basket" of services or prescription formulary.
While the law is generally considered a success and Israeli citizens enjoy a high standard of medical care comparatively, with more competition having been introduced into the field of health care in the country, and order having been brought into what was once a somewhat disorganized system, the law nevertheless does have its critics. First and foremost among the criticisms raised is that the "basket" may not provide enough coverage. To partly address this issue, the HMOs and insurance companies began offering additional "supplementary" insurance to cover certain additional services not included in the basket. However, since this insurance is optional (though usually very modestly priced, costing the equivalent of about US$10 to $20 a month), critics argue that it goes against the spirit of the new law which stressed equality among all citizens with respect to healthcare. Another criticism is that in order to provide universal coverage to all, the tax income base amount (the maximum amount of yearly earnings that are subject to the tax) was set rather high, causing many high-income taxpayers to see the amount they pay for their health premiums (now health tax) skyrocket. Finally, some complain about the constantly rising costs of copayments for certain services.
Macau
Macau offers universally accessible single-payer system funded by taxes. Health care is provided by the Bureau for Health.
People's Republic of China
Since the founding of the People's Republic of China, the goal of health care programs has been to provide care to every member of the population and to make maximum use of limited health-care personnel, equipment, and financial resources.
China is undertaking a reform on its health care system, which was largely privatized in the 1990s. The New Rural Co-operative Medical Care System (NRCMCS), is a new 2005 initiative to overhaul the healthcare system, particularly intended to make it more affordable for the rural poor. Under the NRCMCS, the annual cost of medical coverage is 50 yuan (US$7) per person. Of that, 20 yuan is paid in by the central government, 20 yuan by the provincial government and a contribution of 10 yuan is made by the patient. As of September 2007, around 80% of the whole rural population of China had signed up (about 685 million people). The system is tiered, depending on the location. If patients go to a small hospital or clinic in their local town, the scheme will cover from 70–80% of their bill. If they go to a county one, the percentage of the cost being covered falls to about 60%. And if they need specialist help in a large modern city hospital, they have to bear most of the cost themselves, the scheme would cover about 30% of the bill.[41]
On January 21, 2009, the Chinese government announced that a total of 850 billion yuan (US$127.5 billion) will be provided between 2009 and 2011 in order to improve the existing health care system.[42]
At the end of 2008, the government published its reform plan clarifying government's responsibility by saying that it would play a dominant role in providing public health and basic medical service. It declared "Both central and local governments should increase health funding. The percentage of government's input in total health expenditure should be increased gradually so that the financial burden of individuals can be reduced," The plan listed public health, rural areas, city community health services and basic medical insurance as four key areas for government investment. It also promised to tighten government control over medical fees in public hospitals and to set up a "basic medicine system" to quell public complaints of rising drug costs.[43]
The plan was passed by the Chinese Cabinet in January 2009. The long-awaited medical reform plan promised to spend 850 billion yuan by 2011 to provide universal medical service and that measures would be taken to provide basic medical security to all Chinese.[44]
Singapore
Singapore has a universal health care system where government ensures affordability, largely through compulsory savings and price controls, while the private sector provides most care. Overall spending on health care amounts to only 3% of annual GDP. Of that, 66% comes from private sources.[45] Singapore currently has the second lowest infant mortality rate in the world and among the highest life expectancies from birth, according to the World Health Organization.[46] Singapore has "one of the most successful healthcare systems in the world, in terms of both efficiency in financing and the results achieved in community health outcomes," according to an analysis by global consulting firm Watson Wyatt.[47] Singapore's system uses a combination of compulsory savings from payroll deductions (funded by both employers and workers) a nationalized health insurance plan, and government subsidies, as well as "actively regulating the supply and prices of healthcare services in the country" to keep costs in check; the specific features have been described as potentially a "very difficult system to replicate in many other countries." Many Singaporeans also have supplemental private health insurance (often provided by employers) for services not covered by the government's programs.[47]
Taiwan
The current health care system in Taiwan, known as National Health Insurance (NHI), was instituted in 1995. NHI is a single-payer compulsory social insurance plan which centralizes the disbursement of health care dollars. The system promises equal access to health care for all citizens, and the population coverage had reached 99% by the end of 2004.[48] NHI is mainly financed through premiums, which are based on the payroll tax, and is supplemented with out-of-pocket payments and direct government funding. In the initial stage, fee-for-service predominated for both public and private providers.
NHI delivers universal coverage offered by a government-run insurer. The working population pays premiums split with their employers, others pay a flat rate with government help and the poor or veterans are fully subsidized.[49]
Under this model, citizens have free range to choose hospitals and physicians without using a gatekeeper and do not have to worry about waiting lists. NHI offers a comprehensive benefit package that covers preventive medical services, prescription drugs, dental services, Chinese medicine, home nurse visits and many more. Since NHI, the previously uninsured have increased their usage of medical services. Most preventive services are free such as annual checkups and maternal and child care. Regular office visits have co-payments as low as US $5 per visit. Co-payments are fixed and unvaried by the person's income.[50]
Thailand
Thailand introduced universal coverage reforms in 2001, becoming one of only a handful of lower-middle income countries to do so at the time. Means-tested health care for low income households was replaced by a new and more comprehensive insurance scheme, originally known as the 30 baht project, in line with the small co-payment charged for treatment. People joining the scheme receive a gold card which allows them to access services in their health district, and, if necessary, be referred for specialist treatment elsewhere. The bulk of finance comes from public revenues, with funding allocated to Contracting Units for Primary Care annually on a population basis. According to the WHO, 65% of Thailand's health care expenditure in 2004 came from the government, 35% was from private sources.[45] Although the reforms have received a good deal of critical comment, they have proved popular with poorer Thais, especially in rural areas, and survived the change of government after the 2006 military coup. The then Public Health Minister, Mongkol Na Songkhla, abolished the 30 baht co-payment and made the UC scheme free. It is not yet clear whether the scheme will be modified further under the coalition government that came to power in January 2008.[51][52][53]
Europe
Virtually all of Europe has either publicly sponsored and regulated universal health care or publicly provided universal healthcare. The public plans in some countries provide basic or "sick" coverage only, with their citizens being able to purchase supplemental insurance for additional coverage. Countries with universal health care include Austria, Belarus,[54] Croatia, Czech Republic, Denmark, Finland, France, Germany, Greece, Iceland, Ireland, Italy, Luxembourg, Malta, Moldova,[55] the Netherlands, Norway, Portugal,[56] Romania, Russia, Serbia, Spain, Sweden, Switzerland, Ukraine,[57] and the United Kingdom.[58]
Austria
Healthcare in Austria is universal for residents of Austria as well as those from other EU countries.[59] Austria has a two-tier health care system in which many individuals receive publicly funded care; they also have the option to purchase supplementary private health insurance.
Croatia
Croatia has a universal health care system that provides high quality medical services and is coordinated by the Ministry of Health. The population is covered by a basic health insurance plan provided by statute and optional insurance and administered by the Croatian Health Insurance Fund. In 2012, annual compulsory healthcare related expenditures reached 21.0 billion kunas (c. 2.8 billion euro). There are hundreds of healthcare institutions in Croatia, including 79 hospitals and clinics with 25,285 beds, caring for more than 760 thousand patients per year, 5,792 private practice offices and 79 emergency medical service units.
Czech Republic
Czech Republic has a universal public health system paid largely from taxation. Private health care systems do co-exist freely alongside public ones, sometimes offering better quality or faster service. Almost all medical services are covered by health insurance and insurance companies, though certain services such as prescription drugs or vision and dental care are only covered partially.
Denmark
Denmark has a universal public health system paid largely from taxation with local municipalities delivering health care services in the same way as other Scandinavian countries. Primary care is provided by a general practitioner service run by private doctors contracting with the local municipalities with payment on a mixed per capita and fee for service basis. Most hospitals are run by the municipalities (only 1% of hospital beds are in the private sector).
Finland
In Finland, public medical services at clinics and hospitals are run by the municipalities (local government) and are funded 76% by taxation, 20% by patients through access charges, and 4% by others. Private provision is mainly in the primary care sector. There are a few private hospitals.[60] The main hospitals are either municipally owned (funded from local taxes) or run by the medical teaching universities (funded jointly by the municipalities and the national government). According to a survey published by the European Commission in 2000, Finland's is in the top 4 of EU countries in terms of satisfaction with their hospital care system: 88% of Finnish respondents were satisfied compared with the EU average of 41.3%.[61] Finnish health care expenditures are below the European average.[62] The private medical sector accounts for about 14 percent of total health care spending. Only 8% of doctors choose to work in private practice, and some of these also choose to do some work in the public sector.
Taxation funding is partly local and partly nationally based. The national social insurance institution KELA reimburses part of patients prescription costs and makes a contribution towards private medical costs (including dentistry) if they choose to be treated in the private sector rather than the public sector. Patient access charges are subject to annual caps. For example, GP visits cost €11 per visit with annual €33 cap; hospital outpatient treatment €22 per visit; a hospital stay, including food, medical care and medicines €26 per 24 hours, or €12 if in a psychiatric hospital. After a patient has spent €590 per year on public medical services (including prescription drugs), all treatment and medications thereafter in that year are free.
Finland has a highly decentralized three-level public system of health care and alongside this, a much smaller private health-care system.[63] Overall, the municipalities (funded by taxation, local and national) meet about two thirds of all medical-care costs, with the remaining one third paid by the national insurance system (nationally funded), and by private finance (either employer-funded or met by patients themselves).[63] Private inpatient care forms about 3–4% of all inpatient care.[63] In 1999 only 17 per cent of total funding for health care came from insurance, comprising 14.9% statutory (government) insurance and 2.1% private health insurance. Spectacles are not publicly subsidized at all, although dentistry is available as a municipal service or can be obtained privately with partial reimbursement from the state.[63] The government announced in 2009 that Kela would re-imburse the cost of private dental-hygiene work, starting in 2010.[64]
The percentage of total health expenditure financed by taxation in Finland (78%)[65] is above the OECD average and similar to the levels seen in Germany (77%) and France (80%) but below the level seen in the UK (87%). The quality of service in Finnish health care, as measured by patient satisfaction, is excellent. According to a survey published by the European Commission in 2000, Finland has one of the highest ratings of patient satisfaction with their hospital care system in the EU: 88% of Finnish respondents were satisfied compared with the EU average of 41.3%.[66]
There are caps on total medical expenses that are met out-of-pocket for drugs and hospital treatments. The National Insurance system pays all necessary costs over these caps. Public spending on health care in 2006 was 13.6 billion euros (equivalent to US$338 per person per month). The increase over 2005 at 8.2 per cent was below the OECD average of 9 percent. Household budgets directly met 18.7 per cent of all health-care costs.[67]
France
France has a system of universal health care largely financed by government through a system of national health insurance. It is consistently ranked as one of the best in the world.[68]
Germany
Germany has the world's oldest national social health insurance system,[69][70][71] with origins dating back to Otto von Bismarck's Sickness Insurance Law of 1883.[72][73] The system is decentralized with private practice physicians providing ambulatory care, and independent, mostly non-profit hospitals providing the majority of inpatient care. Approximately 92% of the population is covered by a 'Statutory Health Insurance' plan, which provides a standardized level of coverage through any one of approximately 1100 public or private sickness funds. Standard insurance is funded by a combination of employee contributions, employer contributions and government subsidies on a scale determined by income level. Higher income workers sometimes choose to pay a tax and opt out of the standard plan, in favor of 'private' insurance. The latter's premiums are not linked to income level but instead to health status.[74]
Historically, the level of provider reimbursement for specific services is determined through negotiations between regional physician's associations and sickness funds. Since 1976 the government has convened an annual commission, composed of representatives of business, labor, physicians, hospitals, and insurance and pharmaceutical industries.[75] The commission takes into account government policies and makes recommendations to regional associations with respect to overall expenditure targets. In 1986 expenditure caps were implemented and were tied to the age of the local population as well as the overall wage increases. Although reimbursement of providers is on a fee-for-service basis the amount to be reimbursed for each service is determined retrospectively to ensure that spending targets are not exceeded. Capitated care, such as that provided by U.S. health maintenance organizations, has been considered as a cost containment mechanism but would require consent of regional medical associations, and has not materialized.[76] Copayments were introduced in the 1980s in an attempt to prevent overutilization and control costs. The average length of hospital stay in Germany has decreased in recent years from 14 days to 9 days, still considerably longer than average stays in the U.S. (5 to 6 days).[77][78] The difference is partly driven by the fact that hospital reimbursement is chiefly a function of the number of hospital days as opposed to procedures or the patient's diagnosis. Drug costs have increased substantially, rising nearly 60% from 1991 through 2005. Despite attempts to contain costs, overall health care expenditures rose to 10.7% of GDP in 2005, comparable to other western European nations, but substantially less than that spent in the U.S. (nearly 16% of GDP).[79]
Greece
The Greek healthcare system provides high quality medical services to insured citizens and is coordinated by the Ministry for Health and Social Solidarity. Public health services are provided by the National Healthcare Service, or ESY (Greek: Εθνικό Σύστημα Υγείας, ΕΣΥ). In 2010 there were 35,000 hospital beds and 131 hospitals in the country.
The Greek healthcare system has received high rankings by the World Health Organization, ranked 14th in the overall assessment and 11th in quality of service in a 2000 report by the WHO.
Guernsey / Jersey
The medical care system in the Channel Islands is very similar to that of the UK in that many of the doctors and nurses have been trained from the UK health perspective. There is universal health care for residents of the islands.[80]
Iceland
Iceland has a universal public health system paid largely from taxation with local municipalities delivering health care services in the same way as other Scandinavian countries. Iceland's entire population has equal access to health care services.
Ireland
The public health care system of the Republic of Ireland is governed by the Health Act 2004,[81] which established a new body to be responsible for providing health and personal social services to everyone living in Ireland – the Health Service Executive. The new national health service came into being officially on January 1, 2005; however the new structures are currently in the process of being established as the reform program continues. In addition to the public-sector, there is also a large private health care market.
Isle of Man
The Isle of Man provides universal public health coverage to its residents.[82]
Italy
Italy has a public health care service for all the residents called "Servizio Sanitario Nazionale" or SSN (National Health Service) which is similar to the UK National Health Service. It is publicly run and funded mostly from taxation: some services requires small co-pays, while other services (like the emergency medicine and the general doctor) are completely free of charge. Like the UK, there is a small parallel private health care system, especially in the field of Dental Medicine.
Luxembourg
Luxembourg provides universal health care coverage to all residents (Luxembourgers and foreigners) by the National Health Insurance (CNS - Caisse nationale de santé (French) or National Gesondheetskeess (Luxembourgish)) which is funded by mandatory contributions of employers and the workforce and by government subsidies for insuring jobseekers, the poor and for financing medical infrastructure. It exists as well a mandatory public long-term care insurance.[83][84]
Netherlands
The Netherlands has a dual-level system. All primary and curative care (i.e. the family doctor service and hospitals and clinics) is financed from private compulsory insurance. Long term care for the elderly, the dying, the long term mentally ill etc. is covered by social insurance funded from taxation. According to the WHO, the health care system in the Netherlands was 62% government funded and 38% privately funded as of 2004.[45]
Insurance companies must offer a core universal insurance package for the universal primary, curative care which includes the cost of all prescription medicines. They must do this at a fixed price for all. The same premium is paid whether young or old, healthy or sick. It is illegal in The Netherlands for insurers to refuse an application for health insurance, to impose special conditions (e.g. exclusions, deductibles, co-pays etc., or refuse to fund treatments which a doctor has determined to be medically necessary). The system is 50% financed from payroll taxes paid by employers to a fund controlled by the Health regulator. The government contributes an additional 5% to the regulator's fund. The remaining 45% is collected as premiums paid by the insured directly to the insurance company. Some employers negotiate bulk deals with health insurers and some even pay the employees' premiums as an employment benefit). All insurance companies receive additional funding from the regulator's fund. The regulator has sight of the claims made by policyholders and therefore can redistribute the funds its holds on the basis of relative claims made by policy holders. Thus insurers with high payouts will receive more from the regulator than those with low payouts. Thus insurance companies have no incentive to deter high cost individuals from taking insurance and are compensated if they have to pay out more than might be expected. Insurance companies compete with each other on price for the 45% direct premium part of the funding and try to negotiate deals with hospitals to keep costs low and quality high. The competition regulator is charged with checking for abuse of dominant market positions and the creation of cartels that act against the consumer interests. An insurance regulator ensures that all basic policies have identical coverage rules so that no person is medically disadvantaged by his or her choice of insurer.
Hospitals in the Netherlands are also regulated and inspected but are mostly privately run and not for profit, as are many of the insurance companies. Patients can choose where they want to be treated and have access to information on the internet about the performance and waiting times at each hospital. Patients dissatisfied with their insurer and choice of hospital can cancel at any time but must make a new agreement with another insurer.
Insurance companies can offer additional services at extra cost over and above the universal system laid down by the regulator, e.g. for dental care. The standard monthly premium for health care paid by individual adults is about €100 per month. Persons on low incomes can get assistance from the government if they cannot afford these payments. Children under 18 are insured by the system at no additional cost to them or their families because the insurance company receives the cost of this from the regulator's fund. There is a fixed yearly threshold of €375 for each adult person, excluding first visits for diagnosis to general physicians.
Norway
Norway has a universal public health system paid largely from taxation in the same way as other Scandinavian countries. Norway's entire population has equal access to health care services. The Norwegian health care system is government-funded and heavily decentralized. The health care system in Norway is financed primarily through taxes levied by county councils and municipalities. Dental care is included for children until 18 years old, and is covered for adults for some ailments.[85]
Norway regularly comes top or close to the top of worldwide healthcare rankings.
Portugal
Portugal's National Healthcare Service, known nationally as Serviço Nacional de Saúde (SNS), is a universal and free healthcare service, provided nationwide since 1979, and is available to both Portuguese and foreigner residents. In 2014, Portugal SNS ranked 13th best healthcare service in Europe.[86] The National Medical Emergency Institute (INEM) is the main emergency medical serviced and can be activated by calling 112.
Romania
According to Article 34 of the Constitution of Romania, the state is obliged "to guarantee the protection of healthcare". Romania has a fully universal health care system, which covers up medical check-ups, any surgical interventions, and any post-operator medical care, as well as free or subsidized medicine for a range of diseases. The state is also obliged to fund public hospitals and clinics. Dental care is not funded by the state, although there are public dental clinics in some hospitals, which treat patients free of charge. However, due to inadequate funding and corruption, it is estimated that a third of medical expenses are, in some cases, supported by the patient.[87] Furthermore, Romania spends, per capita, less than any other EU state on medical care.
Russia and Soviet Union
In the Soviet Union, the preferred term was "socialist medicine"; the Russian language has no term to distinguish between "socialist" and "socialized" (other than "public", Rus: obshchestvenniy/общественный, sometimes "collectivized" or "nationalized", Rus: obobshchestvlenniy/обобществленный).[88][89]
Russia in Soviet times (between 1917 and the early 1990s) had a totally socialist model of health care with a centralised, integrated, hierarchically organised with the government providing free health care to all citizens. Initially successful at combating infectious diseases, the effectiveness of the socialized model declined with underinvestment. Despite a doubling in the number of hospital beds and doctors per capita between 1950 and 1980, the quality of care began to decline by the early 1980s and medical care and health outcomes were below western standards.
The new mixed economy Russia has switched to a mixed model of health care with private financing and provision running alongside state financing and provision. The OECD reported that unfortunately, none of this has worked out as planned and the reforms have in many respects made the system worse.[90] The population's health has deteriorated on virtually every measure. The resulting system is overly complex and very inefficient. It has little in common with the model envisaged by the reformers. Although there are more than 300 private insurers and numerous public ones in the market, real competition for patients is rare leaving most patients with little or no effective choice of insurer, and in many places, no choice of health care provider either. The insurance companies have failed to develop as active, informed purchasers of health care services. Most are passive intermediaries, making money by simply channelling funds from regional OMS funds to healthcare providers.
Main source: OECD: Health care reforms in Russia
Article 41 of the Constitution of the Russian Federation confirms a citizen's right to state healthcare and medical assistance free of charge.[91] This is achieved through state compulsory medical insurance (OMS) which is free to Russian citizens, funded by obligatory medical insurance payments made by companies and government subsidies.[92][93] Introduction in 1993 reform of new free market providers in addition to the state-run institutions intended to promote both efficiency and patient choice. A purchaser-provider split help facilitate the restructuring of care, as resources would migrate to where there was greatest demand, reduce the excess capacity in the hospital sector and stimulate the development of primary care. Russian Prime Minister Vladimir Putin announced a new large-scale health care reform in 2011 and pledged to allocate more than 300 billion rubles ($10 billion) in the next few years to improve health care in the country.[94] He also said that obligatory medical insurance tax paid by companies will increase from current 3.1% to 5.1% starting from 2011.[94]
Serbia
The Constitution of the Republic of Serbia states that it is a right of every citizen to seek medical assistance free of charge.[95] This is achieved by mutual contribution to the Compulsory Social Healthcare Fund of RZZO (Republički Zavod za Zdravstveno Osiguranje or National Health Insurance Institution). The amount of contribution depends on the amount of money the person is making. During the 1990s, Serbia's healthcare system has been of a poor quality due to severe underfunding. In the recent years, however, that has changed and the Serbian government has invested heavily in new medical infrastructure, completely remodeling existing hospitals and building two new hospitals in Novi Sad and Kragujevac.
Sweden
Sweden has a universal public health system paid largely from taxation in the same way as other Scandinavian countries. Sweden's entire population has equal access to health care services. The Swedish public health system is funded through taxes levied by the county councils, but partly run by private companies. Government-paid dental care for children under 21 years old is included in the system, and dental care for adults is somewhat subsidised by it.
Sweden also has a smaller private health care sector, mainly in larger cities or as centers for preventive health care financed by employers.
Sweden regularly comes in top in worldwide healthcare rankings.[96]
Switzerland
Healthcare in Switzerland is universal and is regulated by the Federal Health Insurance Act of 1994. Basic health insurance is mandatory for all persons residing in Switzerland (within three months of taking up residence or being born in the country). Insurers are required to offer insurance to everyone, regardless of age or medical condition. They are not allowed to make a profit off this basic insurance, but can on supplemental plans.[97]
United Kingdom
Each of the Countries of the United Kingdom has a National Health Service that provides public healthcare to all UK permanent residents that was originally designed to be free at the point of need and paid for from general taxation; but changes included introducing charging for prescription medicines and dentistry (those below 16 and those on certain benefits may still get free treatment). However, since Health is now a devolved matter, considerable differences are developing between the systems in each of the countries as for example Scotland abolished prescription charges.[98] Private healthcare companies are free to operate alongside the public one.
England
The National Health Service (NHS), created by the National Health Service Act 1946, has provided the majority of healthcare in England since its launch on 5 July 1948.
The NHS Constitution for England documents, at high level, the objectives of the NHS, the legal rights and responsibilities of the various parties (patients, staff, NHS trust boards), and the guiding principles which govern the service.[99] The NHS constitution makes it clear that it provides a comprehensive service, available to all irrespective of age, gender, disability, race, sexual orientation, religion, or belief; that access to NHS services is based on clinical need and not an individual's ability to pay; and that care is never refused on unreasonable grounds. Patient choice in terms of doctor, care, treatments, and place of treatment is an important aspect of the NHS's ambition, and in some cases patients can elect for treatment in other European countries at the NHS's expense. Waiting times are low, with most people able to see their primary care doctor on the same day or the following day.[100] Only 36.1% of hospital admissions are from a waiting list, with the remainder being either emergencies admitted immediately or else pre-booked admissions or the like (e.g., child birth).[101] One of the main goals of care management is to ensure that patients do not experience a delay of more than 18 weeks from initial hospital referral to final treatment, inclusive of time for all associated investigative tests and consultations.[102] At present, two-thirds of patients are treated in under 12 weeks.[103]
Although centrally funded, the NHS is not managed by a large central bureaucracy. Responsibility is highly devolved to geographical areas through Strategic Health Authorities and even more locally through NHS primary care trusts, NHS hospital trusts and increasingly to NHS foundation trusts which are providing even more decentralized services within the NHS framework, with more decision making taken by local people, patients, and staff. The central government office, the Department of Health, is not involved in day-to-day decision making in either the Strategic Health Authorities or the individual local trusts (primarily health, hospital, or ambulance) or the national specialist trusts such as NHS Blood and Transplant, but it does lay down general guidelines for them to follow. Local trusts are accountable to their local populations, whilst government ministers are accountable to Parliament for the service overall.
The NHS provides, among other things, primary care, in-patient care, long-term healthcare, psychiatric care and treatments, ophthalmology, and dentistry. All treatment is free with the exception of certain charges for prescriptions, dentistry and ophthalmology (which themselves are free to children, certain students in full-time education, the elderly, the unemployed and those on low incomes). Around 89 pc of NHS prescriptions are obtained free of charge, mostly for children, pensioners, and pregnant women. Others pay a flat rate of £8.20,[104] and others may cap their annual charges by purchasing an NHS Prescription Prepayment Certificate. Private health care has continued parallel to the NHS, paid for largely by private insurance. Private insurance accounts for only 4 percent of health expenditure and covers little more than a tenth of the population.[105] Private insurers in the UK only cover acute care from specialists. They do not cover generalist consultations, pre-existing conditions, medical emergencies, organ transplants, chronic conditions such as diabetes, or conditions such as pregnancy or HIV.[106]
Most NHS general practitioners are private doctors who contract to provide NHS services, but most hospitals are publicly owned and run through NHS Trusts. A few NHS medical services (such as "surgicentres") are sub-contracted to private providers[107] as are some non-medical services (such as catering). Some capital projects such as new hospitals have been funded through the Private Finance Initiative, enabling investment without (in the short term) increasing the public sector borrowing requirement, because long-term contractually obligated PFI spending commitments are not counted as government liabilities.
Northern Ireland
Health and Social Care in Northern Ireland is the designation of the national public health service in Northern Ireland.
Scotland

NHS Scotland, created by the National Health Service (Scotland) Act 1947, was also launched on 5 July 1948, although it has always been a separate organization. Since devolution, NHS Scotland has followed the policies and priorities of the Scottish Government, including the phasing out of all prescription charges by 2011.
Wales
NHS Wales was originally formed as part of the same NHS structure created by the National Health Service Act 1946 but powers over the NHS in Wales came under the Secretary of State for Wales in 1969,[108] in turn being transferred under devolution to what is now the Welsh Government.
North America
The Bahamas, Barbados, Canada, Costa Rica, Cuba, Mexico, Panama, and Trinidad and Tobago all provide some level of universal health coverage.
The Bahamas
The Bahamas approved the National Health Insurance Act in August 2016. The legislation allows for the establishment of a universal health coverage system that will begin with universal coverage of primary health care services and later expand to include a wide set of benefits including all specialized care. The system will all for universal coverage of a basic benefit package and for voluntary insurance to be purchased as a top up policy to cover services or amenities that are not included in the government plan.[109]
Canada
In 1984, the Canada Health Act was passed, which prohibited extra billing by doctors on patients while at the same time billing the public insurance system. In 1999, the prime minister and most premiers reaffirmed in the Social Union Framework Agreement that they are committed to health care that has "comprehensiveness, universality, portability, public administration and accessibility."[110]
The system is for the most part publicly funded, yet most of the services are provided by private enterprises or private corporations, although most hospitals are public. Most doctors do not receive an annual salary, but receive a fee per visit or service.[111] About 29% of Canadians' health care is paid for by the private sector or individuals.[112] This mostly goes towards services not covered or only partially covered by Medicare such as prescription drugs, dentistry and vision care.[113] Many Canadians have private health insurance, often through their employers, that cover these expenses.[114]
The Canada Health Act of 1984 "does not directly bar private delivery or private insurance for publicly insured services," but provides financial disincentives for doing so. "Although there are laws prohibiting or curtailing private health care in some provinces, they can be changed," according to a report in the New England Journal of Medicine.[115][116] The legality of the ban was considered in a decision of the Supreme Court of Canada which ruled in Chaoulli v. Quebec that "the prohibition on obtaining private health insurance, while it might be constitutional in circumstances where health care services are reasonable as to both quality and timeliness, is not constitutional where the public system fails to deliver reasonable services." The appellant contended that waiting times in Quebec violated a right to life and security in the Quebec Charter of Human Rights and Freedoms. The Court agreed, but acknowledged the importance and validity of the Canada Health Act, and at least four of the seven judges explicitly recognized the right of governments to enact laws and policies which favour the public over the private system and preserve the integrity of the public system.
Costa Rica
Universal healthcare and pensions are run by the Caja Costarricense de Seguro Social (CCSS). In 1941, Costa Rica established Caja Costarricense de Seguro Social (CCSS), a social security insurance system for wage-earning workers. In 1961, coverage was expanded to include workers’ dependents and from 1961 to 1975, a series of expansions extended coverage for primary care and outpatient and inpatient specialized services to people in rural areas, the low-income population, and certain vulnerable populations. Further expansions during the late 1970s extended insurance coverage to farmers, peasants, and independent contract workers. Additionally, CCSS mandates free health service provision to mothers, children, indigenous people, the elderly, and people living with disabilities, regardless of insurance coverage. By 2000, 82 percent of the population was eligible for CCSS, which has continued to expand in the ensuing period. By covering all population groups through the same system, Costa Rica has avoided social insurance stratification and inequity common in many other countries in the region.[117]
CCSS is funded by a 15 percent payroll tax, as well as payments from retiree pensions [6]. Taxes on luxury goods, alcohol, soda, and imported products also help to cover poor households who do otherwise pay into the system. All CCSS funds are merged into a single pool, which is managed by the central financial administration of CCSS. In 1973, the Ministry of Health decided to move away from direct service provision and adopt a steering role. Responsibility for the provision of most care was transferred to the CCSS, although the Ministry retained responsibility for disease control, food and drug regulation, environmental sanitation, child nutrition, and primary care for the poor. Through the CCSS, health care is now essentially free to nearly all Costa Ricans. Private health care is also widely available and INS offers private health insurance plans to supplement CCSS insurance.[118]
Cuba
The Cuban government operates a national health system and assumes fiscal and administrative responsibility for the health care of all its citizens. There are no private hospitals or clinics as all health services are government-run. The present Minister for Public Health is Roberto Morales Ojeda. However, although the coverage is wide, the system is underfunded and recently also understaffed. The government organized medical missions in other countries has taken a very significant amount of doctors and other personal. In 2005 there were 25,000 Cuban doctors in Venezuela.
Mexico
Public health care delivery is accomplished via an elaborate provisioning and delivery system instituted by the Mexican Federal Government. Public health care is provided to all Mexican citizens as guaranteed via Article 4 of the Constitution. Public care is either fully or partially subsidized by the federal government, depending on the person's (Spanish: derechohabiente's) employment status. All Mexican citizens are eligible for subsidized health care regardless of their work status via a system of health care facilities operating under the federal Secretariat of Health (formerly the Secretaria de Salubridad y Asistencia, or SSA) agency. Employed citizens and their dependents, however, are further eligible to use the health care program administered and operated by the Instituto Mexicano del Seguro Social (IMSS) (English: Mexican Social Security Institute). The IMSS health care program is a tripartite system funded equally by the employee, its private employer, and the federal government. The IMSS does not provide service to employees of the public sector. Employees in the public sector are serviced by the Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado (ISSSTE) (English: Institute for Social Security and Services for State Workers), which attends to the health and social care needs of government employees. This includes local, state, and federal government employees. The government of the states in Mexico also provide health services independently of those services provided by the federal government programs. In most states, the state government has established free or subsidized healthcare to all their citizens.
On December 1, 2006, the Mexican government created the Health Insurance for a New Generation also known as "life insurance for babies".[119][120][121] On May 16, 2009, Mexico to Achieve Universal Health Coverage by 2011.[122] On May 28, 2009, Mexico announced Universal Care Coverage for Pregnant Women.[123] On August 2012 Mexico installed a universal healthcare system.[124]
Trinidad and Tobago
A universal health care system is used in Trinidad and Tobago and is the primary form of health-care available in the country. It is used by the majority of the population seeking medical assistance, as it is free for all citizens.
United States
| This article is part of a series on |
| Healthcare reform in the United States of America |
|---|
 |
|
|
Third-party payment models |
|
|
The United States does not have a universal health care system. However, the Patient Protection and Affordable Care Act (PPACA) as amended by the Health Care and Education Reconciliation Act of 2010, seeks to have expanded insurance coverage to legal residents by 2014. It provides for federally mandated health insurance to be implemented in the United States during the 2010–2019 decade with the Federal government subsidizing legal resident households with income up to 400% of the Federal poverty level.[125] This threshold varies according to State and household size, but for an average family of four, subsidies would be available for families whose income was about $88,000 or lower.[126] In June 2010 adults with pre-existing conditions became eligible to join a temporary high-risk pool.[127] In 2014, applicants of the same age began to be able to obtain health insurance at the same published rate regardless of health status — the first time in U.S. history that insurers no longer had the right to load the premium or deny coverage prior to contract, or cancel a policy after contract due to an adverse health condition, or test result indicating that one may be imminent. The law prohibits insurers from capping their liability for a person's health care needs, a move which is expected to rectify medically induced bankruptcy. As of April 13, 2015, the U.S. uninsured rate fell to 11.9% from the 17.1% recorded at the end of the fourth quarter of 2013. This is the lowest quarterly average recorded since Gallup and Healthways began tracking the percentage of uninsured Americans in 2008. Gallup attributed this sharp decline to the Affordable Care Act's requirements for most Americans to have healthcare in the beginning of the first quarter of 2014.[128]
The Congressional Budget Office and related government agencies scored the cost of a universal health care system several times since 1991, and have uniformly predicted cost savings,[129] partly from the elimination of insurance company overhead costs.[130] In 2009, a universal health care proposal was pending in Congress, the United States National Health Care Act (H.R. 676, formerly the "Medicare for All Act").
The Congressional Budget Office (CBO) estimated that the bill would reduce the number of nonelderly people who are uninsured by about 32 million, leaving about 23 million nonelderly residents uninsured (about one-third of whom would be illegal immigrants). Under the legislation, the share of legal nonelderly residents with insurance coverage would rise from about 83 percent in 2010 to about 94 percent by 2019.[131]
In May 2011, the state of Vermont became the first state to pass legislation establishing a single-payer health care system. The legislation, known as Act 48, establishes health care in the state as a "human right" and lays the responsibility on the state to provide a health care system which best meets the needs of the citizens of Vermont. The proposal was shelved not long after the main provisions of the law took effect in 2014.[132] A revised estimate in July 2012 by the CBO stated 30 million people would gain access to health insurance under the law.[133]
Discussion in the United States commonly uses the term socialized medicine to impart a pejorative meaning to the idea of universal health care.
South America
Argentina, Brazil, Chile, Colombia, Peru, Uruguay, and Venezuela all have public universal health care provided.
Argentina
Health care is provided through a combination of employer and labor union-sponsored plans (Obras Sociales), government insurance plans, public hospitals and clinics and through private health insurance plans. It costs almost 10% of GDP and is available to anyone regardless of ideology, beliefs, race or nationality.
Brazil
The universal health care system was adopted in Brazil in 1988 after the end of the military regime's rule. However, universalized/socialized health care was available many years before, in some cities, once the 27th amendment to the 1969 Constitution imposed the duty of applying 6% of their income in healthcare on the municipalities.[134]
Chile
Health care in Chile is provided by the government (via Fonasa) and by private insurers (via Isapre). All workers and pensioners are mandated to pay 7% of their income for health care insurance (the poorest pensioners are exempt from this payment). Workers who choose not to join an Isapre, are automatically covered by Fonasa. Fonasa also covers unemployed people receiving unemployment benefits, uninsured pregnant women, insured worker's dependant family, people with mental or physical disabilities and people who are considered poor or indigent.
Fonasa costs vary depending on income, disability or age. Attention at public health facilities via Fonasa is free for low-income earners, people with mental or physical disabilities and people over the age of 60. Others pay 10% or 20% of the costs, depending on income and number of dependants. Fonasa beneficiaries may also seek attention in the private sector, for a designated fee.
Additionally, there are a number of high-mortality illnesses (currently 69) that have special attention guarantees for both Isapre and Fonasa affiliates, in relation to access to treatment, waiting times, maximum costs and quality of service.
Colombia
In 1993 a reform transformed the health care system in Colombia, trying to provide a better, sustainable, health care system and to reach every Colombian citizen.
Peru
On April 10, 2009, the Government of Peru published the Law on Health Insurance to enable all Peruvians to access quality health services, and contribute to regulate the financing and supervision of these services. The law enables all population to access diverse health services to prevent illnesses, and promote and rehabilitate people, under a Health Basic Plan (PEAS).[135][136]
On April 2, 2010, President Alan Garcia Perez on Friday signed a supreme ordinance approving the regulations for the framework law on the Universal Health Insurance, which seeks to provide access to quality health care for all Peruvian citizens.
Peru's Universal Health Insurance law aims to increase access to timely and quality health care services, emphasizes maternal and child health promotion, and provides the poor with protection from financial ruin due to illness.[137]
The regulation states that membership of the Universal Health Insurance (AUS for its Spanish acronym) is compulsory for the entire population living in the country. To that end, the Ministry of Health will approve, by supreme ordinance, the mechanisms leading to compulsory membership, as well as escalation and implementation.[138]
Oceania
Australia and New Zealand have universal health care.
Australia

In Australia, Medibank — as it was then known — was introduced, by the Whitlam Labor government on July 1, 1975, through the Health Insurance Act 1973. The Australian Senate rejected the changes multiple times and they were passed only after a joint sitting after the 1974 double dissolution election. However, Medibank was supported by the subsequent Fraser Coalition (Australia) government and became a key feature of Australia's public policy landscape. The exact structure of Medibank/Medicare, in terms of the size of the rebate to doctors and hospitals and the way it has administered, has varied over the years. The original Medibank program proposed a 1.35% levy (with low income exemptions) but these bills were rejected by the Senate, and so Medibank was funded from general taxation. In 1976, the Fraser Government introduced a 2.5% levy and split Medibank in two: a universal scheme called Medibank Public and a government-owned private health insurance company, Medibank Private.
During the 1980s, Medibank Public was renamed Medicare by the Hawke Labor government, which also changed the funding model, to an income tax surcharge, known as the Medicare Levy, which was set at 1.5%, with exemptions for low income earners.[139] The Howard Coalition government introduced an additional levy of 1.0%, known as the Medicare Levy Surcharge, for those on high annual incomes ($70,000) and do not have adequate levels of private hospital coverage.[140] This was part of an effort by the Coalition to encourage take-up of private health insurance. According to WHO, government funding covered 67.5% of Australia's health care expenditures in 2004; private sources covered the remaining 32.5% of expenditures.[45]
New Zealand
As with Australia, New Zealand's healthcare system is funded through general taxation. According to the WHO, government sources covered 77.4% of New Zealand's health care costs in 2004; private expenditures covered the remaining 22.6%.[45]
See also
References
- ↑ Stuckler, David; Feigl, Andrea B.; Basu, Sanjay; McKee, Martin (November 2010). "The political economy of universal health coverage. Background paper for the First Global Symposium on Health Systems Research, 16–19 November 2010, Montreaux, Switzerland" (PDF). Pacific Health Summit. Seattle: National Bureau of Asian Research. p. 16.
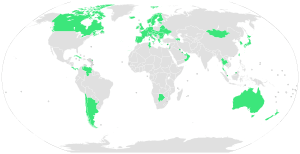
Figure 2. Global Prevalence of Universal Health Care in 2009; 58 countries: Andorra, Antigua, Argentina, Armenia, Australia, Austria, Azerbaijan, Bahrain, Belarus, Belgium, Bosnia and Herzegovina, Botswana, Brunei Darussalam, Bulgaria, Canada, Chile, Costa Rica, Croatia, Cuba, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Israel, Italy, Japan, Kuwait, Luxembourg, Moldova, Mongolia, Netherlands, New Zealand, Norway, Oman, Panama, Portugal, Romania, Singapore, Slovakia, Slovenia, South Korea, Spain, Sweden, Switzerland, Taiwan, Thailand, Tunisia, UAE, Ukraine, United Kingdom, Venezuela.
- ↑ "International Health Comparisons: A Compendium of published information on healthcare systems, the provision of health care and health achievement in 10 countries". Retrieved October 15, 2013.
- ↑ "Snapshots of Health Systems: The state of affairs in 16 countries in summer 2004 WHO" (PDF). Archived from the original (PDF) on 2010-01-25.
- ↑ Tran, Mark (December 13, 2012), "Global development,Health (Society),Society,United Nations (News),World news", The Guardian, London
- ↑ "Algeria – Health And Welfare". Countrystudies.us. Retrieved November 14, 2011.
- ↑ http://www.marines.mil/Portals/59/Publications/Algeria%20Profile.pdf
- ↑ "Botswana:The Health System - AHO". Retrieved November 30, 2016.
- ↑ JLN. "Burkina Faso adopts universal health insurance system - Joint Learning Network". Retrieved November 30, 2016.
- ↑ "Insurance". Retrieved November 30, 2016.
- ↑ "NHIS - Your Access to Healthcare". Retrieved November 30, 2016.
- ↑ "Tiny African Island Has Soaring GDP, Free Healthcare and Free Higher Education - The Utopianist". Retrieved November 30, 2016.
- ↑ "International Journal for Equity in Health | Full text | Social inequalities and health inequity in Morocco". Equityhealthj.com. Retrieved November 14, 2011.
- ↑ "In Rwanda, Health Care Coverage That Eludes the U.S.". Opinionator (blog of The New York Times). Archived from the original on 2014-02-03.
- ↑ "Health care in South Africa". SouthAfrica.info. Retrieved November 14, 2011.
- ↑ "The healthcare system in Tunisia". Retrieved November 30, 2016.
- ↑ "National Health Policy: Ministry of Health" (PDF).
- ↑ "Introduction to healthcare in Bahrain". Justlanded.com. Retrieved November 14, 2011.
- ↑ Health care in Iran
- ↑ The Health Care System in Israel- An Historical Perspective Israel Ministry of Foreign Affairs. Retrieved June 7, 2006.
- ↑ "Embassy of Jordan (Washington, D.C.) – Jordan Information Bureau". Jordanembassyus.org. Retrieved November 14, 2011.
- ↑ "Kazakhstan Health System – Flags, Maps, Economy, History, Climate, Natural Resources, Current Issues, International Agreements, Population, Social Statistics, Political System". Photius.com. Retrieved November 14, 2011.
- ↑ "Malaysia Health System Review" (PDF).
- ↑ "Mongolia Health-Care Systems – Flags, Maps, Economy, History, Climate, Natural Resources, Current Issues, International Agreements, Population, Social Statistics, Political Sy". Photius.com. Retrieved November 14, 2011.
- ↑ "Oman Guide: Introduction, An introduction to health care in Oman: Oman offers high quality health care equal". Justlanded.com. Retrieved November 14, 2011.
- ↑ "WHO | Primary Health Care in Action". Who.int. September 26, 2008. Retrieved November 14, 2011.
- ↑ "''Ministry of Health and Nutrition, Sri Lanka''". Health.gov.lk. Retrieved November 14, 2011.
- ↑ Obaida Hamad (February 2011). "Health system reforms: Better services at what cost?". Forward Magazine.
- ↑ "''Bureau of National Health Insurance, Taiwan''". Nhi.gov.tw. September 28, 2011. Retrieved November 14, 2011.
- ↑ "Tajikistan Health Care System – Flags, Maps, Economy, History, Climate, Natural Resources, Current Issues, International Agreements, Population, Social Statistics, Political S". Photius.com. Retrieved November 14, 2011.
- ↑ "Health Care in Turkey". All About Turkey. November 20, 2006. Retrieved November 14, 2011.
- ↑ "Turkmenistan Structure of Health Care – Flags, Maps, Economy, History, Climate, Natural Resources, Current Issues, International Agreements, Population, Social Statistics, Pol". Photius.com. Retrieved November 14, 2011.
- ↑ "Country Health System Profile: Bhutan". World Health Organization. Archived from the original on 2012-06-01.
- ↑ "Healthy life expectancy in Hong Kong". World Health Organization. Retrieved June 7, 2008.
- ↑ "Rank Order – Life expectancy at birth". The World Factbook, Central Intelligence Agency. January 24, 2008. Retrieved February 1, 2008.
- ↑ "World Population Prospects: The 2006 Revision" (PDF). United Nations. 2007. Retrieved February 1, 2008.
- ↑ "Live Donor Liver Transplantation: Current Status" (PDF). Springerlink.com. Retrieved November 14, 2011.
- ↑ "Modi's ambitious health policy may dwarf Obamacare". Retrieved November 30, 2016.
- ↑ "Rajiv Gandhi Jeevandayee Arogya Yojana". Government of Maharashtra. 16 January 2016. Retrieved 16 January 2016.
- ↑ Kalra, Aditya. "India's universal healthcare rollout to cost $26 billion". Retrieved November 30, 2016.
- ↑ "history of Israel health care".
- ↑ Carrin G, Ron A, Hui Y, et al. (April 1999). "The reform of the rural cooperative medical system in the People's Republic of China: interim experience in 14 pilot counties". Soc Sci Med. 48 (7): 961–72. doi:10.1016/S0277-9536(98)00396-7. PMID 10192562.
- ↑ 3年內醫改投入8500億. Retrieved January 21, 2009.
- ↑ Staff (October 14, 2008). "Medical Reform Draft Open to Public Debate". Xinhua News Agency (via the China Internet Information Center). Retrieved April 10, 2014.
- ↑ Staff (January 21, 2009). "China Passes New Medical Reform Plan". xinhuanet.com. Retrieved April 10, 2014.
- 1 2 3 4 5 "World Health Organization Statistical Information System: Core Health Indicators". Who.int. Retrieved November 14, 2011.
- ↑ World Health Organization, "World Health Statistics 2007: Mortality", based on 2005 data.
- 1 2 John Tucci, "The Singapore health system – achieving positive health outcomes with low expenditure", Watson Wyatt Healthcare Market Review, October 2004. Archived April 19, 2010, at the Wayback Machine.
- ↑ Fanchiang, Cecilia (January 2, 2004). "New IC health insurance card expected to offer many benefits" Archived June 6, 2008, at the Wayback Machine.. Taiwan Journal. Retrieved March 28, 2008.
- ↑ "Taiwan Takes Fastrack to Universal Health Care". All Things Considered, NPR. April 15, 2008. Retrieved October 5, 2008.
- ↑ Jui-Fen Rachel Lu; William C. Hsiao (2003). "Does Universal Health Insurance Make Health Care Unaffordable? Lessons From Taiwan". Health Affairs. 22 (3): 77–88. doi:10.1377/hlthaff.22.3.77. PMID 12757274.
- ↑ G20 Health Care: "Health Care Systems and Health Market Reform in the G20 Countries." Prepared for the World Economic Forum by Ernst & Young. January 3, 2006.
- ↑ "''The Universal Coverage Policy of Thailand: An Introduction''". Unescap.org. Retrieved November 14, 2011.
- ↑ Hughes D, Leethongdee S (2007). "Universal coverage in the land of smiles: lessons from Thailand's 30 baht health reforms". Health Affairs. 26 (4): 999–1008. doi:10.1377/hlthaff.26.4.999. PMID 17630443.
- ↑ Belarus. "Health in Belarus. Healthcare system of Belarus". Europe-cities.com. Retrieved November 14, 2011.
- ↑ Moldova Healthcare Archived January 25, 2010, at the Wayback Machine.
- ↑ Portugal: Bentes M, Dias CM, Sakellarides C, Bankauskaite V. Health Care Systems in Transition: Portugal. WHO are Regional Offices for Europe on behalf of the European Observatory on Health Systems and Policies, 2004.
- ↑ Constitution of Ukraine Chapter 2, Article 49. Adopted at the Fifth Session of the Verkhovna Rada of Ukraine on June 28, 1996.
- ↑ Physicians for a National Health Program "International Health Systems".
- ↑ Staff (undated). "The Austrian healthcare system Overview of how it works". justlanded.com. Retrieved October 16, 2011.
- ↑ "KELA – Use of European Health Insurance Card in Finland". Kela.fi. Retrieved November 14, 2011.
- ↑ "European Commission: Health and long-term care in the European Union" (PDF). Retrieved November 14, 2011.
- ↑ "Health Systems in Transition Vol. 10 No. 4 2008; Finland health system review" (PDF). Retrieved January 9, 2015. line feed character in
|title=at position 29 (help) - 1 2 3 4 Järvelin, Jutta (2002). "Health Care Systems in Transition" (PDF). The European Observatory on Health Care Systems. Retrieved February 25, 2009.
- ↑ Kela publication to all households 2009.
- ↑ http://www.oecd.org/dataoecd/52/33/38976604.pdf
- ↑ http://ec.europa.eu/public_opinion/archives/ebs/ebs_283_en.pdf European Commission: Health and long-term care in the European Union
- ↑ "News item on healthcare costs in 2006 (in Finnish)".
- ↑ "World Health Organization Assesses the World's Health Systems". Who.int. 8 December 2010. Retrieved 6 January 2012.
- ↑ Bump, Jesse B. (October 19, 2010). "The long road to universal health coverage. A century of lessons for development strategy" (PDF). Seattle: PATH. Retrieved March 11, 2013.
Carrin and James have identified 1988—105 years after Bismarck's first sickness fund laws—as the date Germany achieved universal health coverage through this series of extensions to minimum benefit packages and expansions of the enrolled population. Bärnighausen and Sauerborn have quantified this long-term progressive increase in the proportion of the German population covered by public and private insurance. Their graph is reproduced below as Figure 1: German Population Enrolled in Health Insurance (%) 1885–1995.
- ↑ Carrin, Guy; James, Chris (January 2005). "Social health insurance: Key factors affecting the transition towards universal coverage" (PDF). International Social Security Review. 58 (1): 45–64. doi:10.1111/j.1468-246x.2005.00209.x. Retrieved March 11, 2013.
Initially the health insurance law of 1883 covered blue-collar workers in selected industries, craftspeople and other selected professionals.6 It is estimated that this law brought health insurance coverage up from 5 to 10 per cent of the total population.
- ↑ Bärnighausen, Till; Sauerborn (May 2002). "One hundred and eighteen years of the German health insurance system: are there any lessons for middle- and low income countries?" (PDF). Social Science & Medicine. 54 (10): 1559–1587. doi:10.1016/S0277-9536(01)00137-X. PMID 12061488. Retrieved March 11, 2013.
As Germany has the world's oldest SHI [social health insurance] system, it naturally lends itself to historical analyses.
|first3=missing|last3=in Authors list (help) - ↑ Leichter, Howard M. (1979). A comparative approach to policy analysis: health care policy in four nations. Cambridge: Cambridge University Press. p. 121. ISBN 0-521-22648-1.
The Sickness Insurance Law (1883). Eligibility. The Sickness Insurance Law came into effect in December 1884. It provided for compulsory participation by all industrial wage earners (i.e., manual laborers) in factories, ironworks, mines, shipbuilding yards, and similar workplaces.
- ↑ Hennock, Ernest Peter (2007). The origin of the welfare state in England and Germany, 1850–1914: social policies compared. Cambridge: Cambridge University Press. p. 157. ISBN 978-0-521-59212-3.
- ↑ GmbH, Finanztip Verbraucherinformation gemeinnützige. "Finanztip : Finanztip – Das gemeinnützige Verbraucherportal". Retrieved November 30, 2016.
- ↑ Kirkman-Liff BL (1990). "Physician Payment and Cost-Containment Strategies in West Germany: Suggestions for Medicare Reform". Journal of Health Care Politics, Policy and Law (Duke University). 15 (1): 69–99. doi:10.1215/03616878-15-1-69. PMID 2108202.
- ↑ Henke KD (May 2007). "[External and internal financing in health care]". Med. Klin. (Munich) (in German). 102 (5): 366–72. doi:10.1007/s00063-007-1045-0. PMID 17497087.
- ↑ "Length of hospital stay, Germany". Group-economics.allianz.com. July 25, 2005. Retrieved November 14, 2011.
- ↑ "Length of hospital stay, U.S". Cdc.gov. Retrieved November 14, 2011.
- ↑ Borger C, Smith S, Truffer C, et al. (2006). "Health spending projections through 2015: changes on the horizon". Health Aff (Millwood). 25 (2): w61–73. doi:10.1377/hlthaff.25.w61. PMID 16495287.
- ↑ "Expat Guernsey". Retrieved August 7, 2011.
- ↑ "Health Act 2004". Irish Statute Book. Office of the Attorney General. Retrieved October 5, 2010.
- ↑ <Please add first missing authors to populate metadata.>. "Department of Health Service Delivery Plan 2011" (PDF). Retrieved August 7, 2011.
- ↑ "Life rsciences & health care in Luxembourg".
- ↑ "Législation-Code de la sécurité sociale & Statuts de la Caisse nationale de santé".
- ↑ "Who Pays Your Dental Bill?". Helsenorge.
- ↑ http://www.healthpowerhouse.com/files/EHCI_2014/EHCI_2014_report.pdf
- ↑ "Bribes in hospitals: "tariff" for a surgery or a C-cut".
- ↑ Zhuraleva et al., Teaching History of Medicine in Russia.
- ↑ Yandex Lingvo
- ↑ "Search Official Documents - OECD" (PDF). Retrieved November 30, 2016.
- ↑ "The Constitution of the Russian Federation".
- ↑ "О МЕДИЦИНСКОМ СТРАХОВАНИИ ГРАЖДАН В РОССИЙСКОЙ ФЕДЕРАЦИИ".
- ↑ "Russia – Unified Social Tax replaced by insurance contributions". Archived from the original on June 28, 2010.
- 1 2 "Putin says Russia needs major health care reform".
- ↑ "Ustav Republike Srbije (The Constitution of the Republic of Serbia)".
- ↑ "How the NHS could learn from Sweden". BBC News. November 28, 2005. Retrieved September 15, 2009.
- ↑ Schwartz, Nelson D. (October 1, 2009). "Swiss health care thrives without public option". The New York Times. p. A1.
- ↑ NHS now four different systems BBC January 2, 2008
- ↑ "NHS Constitution for England". Dh.gov.uk. Retrieved 2011-11-14.
- ↑ Cathy Schoen and Robin Osborn (2004). "The Commonwealth Fund 2004 International Health Policy Survey of Primary Care in Five Countries" (PDF).
- ↑ Kingdom, NHS Digital, 1 Trevelyan Square, Boar Lane, Leeds, LS1 6AE, United. "Hospital Episode Statistics" (PDF). Retrieved November 30, 2016.
- ↑ "18 weeks patient pathway". Retrieved November 30, 2016.
- ↑ "18 weeks patient pathway" (PDF). Retrieved November 30, 2016.
- ↑ "NHS charges to rise in England". BBC News. 5 March 2009. Retrieved 2011-11-14.
- ↑ Smee, Clive (October 2000). "Department of Health Special Section: Reconsidering the Role of Competition in Health Care Markets". Journal of Health Politics, Policy and Law. 25 (5): 945–951.
- ↑ Are you buying private medical insurance? Association of British Insurers
- ↑ "N. generation surgery-centers to carry out thousands more NHS operations every year". Department of Health. 3 December 2002. Retrieved 2006-09-15.
- ↑ Introduction to NHS Wales 1960's www.wales.nhs.uk
- ↑ "NHI Bahamas -". Retrieved November 30, 2016.
- ↑ Government of Canada, Social Union, News Release, "A Framework to Improve the Social Union for Canadians: An Agreement between the Government of Canada and the Governments of the Provinces and Territories, February 4, 1999." Retrieved December 20, 2006.
- ↑ Public vs. private health care. CBC, December 1, 2006.
- ↑ Press release, "Health care spending to reach $160 billion this year", Canadian Institute for Health Information, November 13, 2007. Retrieved November 19, 2007.
- ↑ National Health Expenditure Trends, 1975–2007, Canadian Institute for Health Information, November 13, 2007. Retrieved November 19, 2007.
- ↑ The OECD Health Project (2004). Private Health Insurance In OECD Countries. Organisation for Economic Co-operation and Development. ISBN 92-64-00668-0.
- ↑ Kraus, Clifford (February 26, 2006). "As Canada's Slow-Motion Public Health System Falters, Private Medical Care Is Surging". The New York Times. Retrieved July 16, 2007.
- ↑ Steinbrook, R. (April 2006). "Private health care in Canada". New England Journal of Medicine. 354 (16): 1661–4. doi:10.1056/NEJMp068064. PMID 16625005.
- ↑ "Health System Innovations in Central America". The World Bank. July 1, 2005. doi:10.1596/978-0-8213-6278-5. Retrieved November 30, 2016 – via elibrary.worldbank.org (Atypon).
- ↑ Toward Universal Health Coverage and Equity in Latin America and the Caribbean http://dx.doi.org/10.1596/978-1-4648-0454-0
- ↑ Message to the Nation from the President of Mexico, Felipe Calderón Hinojosa, on the occasion of his first State of the Union Address Archived December 8, 2009, at the Wayback Machine.
- ↑ President Calderón during First National Week of Affiliation to Medical Insurance for a New Generation Archived January 10, 2011, at the Wayback Machine.
- ↑ President Calderón at Launching of Affiliation to Medical Insurance for a New Generation Archived June 22, 2009, at the Wayback Machine.
- ↑ Mexico to Achieve Universal Health Coverage by 2011 Archived June 22, 2009, at the Wayback Machine.
- ↑ International Women's Day Archived June 22, 2009, at the Wayback Machine.
- ↑ "Mexico achieves universal health coverage, enrolls 52.6 million people in less than a decade". Harvard School of Public Health. August 15, 2012. Retrieved September 16, 2013.
- ↑ "5 key things to remember about health care reform". CNN. March 25, 2010.
- ↑ "2009 Poverty Guideline Computations". Aspe.hhs.gov. Retrieved November 14, 2011.
- ↑ Grier, Peter (March 24, 2010). "Health care reform bill 101: rules for preexisting conditions". The Christian Science Monitor. Retrieved March 25, 2010.
- ↑ "In U.S., Uninsured Rate Dips to 11.9% in First Quarter". Gallup.
- ↑ Physicians for a National Health Program (January, 2008) "Single Payer System Cost?" pnhp.org
- ↑ Levy A.R., et al. (2010). "International comparison of comparative effectiveness research in five jurisdictions: insights for the US". PharmacoEconomics. 28 (10): 813–30. doi:10.2165/11536150-000000000-00000. PMID 20831289.
- ↑ "Cost Estimate for Pending Health Care Legislation". CBO Director's Blog. Retrieved March 21, 2010.
- ↑ "Why single payer died in Vermont". Retrieved November 30, 2016.
- ↑ http://www.cbo.gov/sites/default/files/cbofiles/attachments/43471-hr6079.pdf
- ↑ "Emc1". Planalto.gov.br. Retrieved November 14, 2011.
- ↑ "Law on Health Insurance published today". Andina.com.pe. Retrieved November 14, 2011.
- ↑ "President Garcia: Law on Health Insurance marks major reform". Andina.com.pe. Retrieved November 14, 2011.
- ↑ "Aseguramiento Universal de Salud – Perú". Aus-peru.blogspot.com. February 24, 2004. Retrieved November 14, 2011.
- ↑ "President Garcia signs regulations for Universal Health Insurance law". Andina.com.pe. Retrieved November 14, 2011.
- ↑ Australian Taxation Office (June 19, 2007). "What is the Medicare levy?". Archived from the original on October 22, 2007. Retrieved February 15, 2008.
- ↑ "Medicare Levy Surcharge". Ato.gov.au. Retrieved November 14, 2011.
.jpg)
Aug2005.jpg)