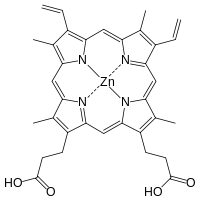
Zinc protoporphyrin
 | |
| Names | |
|---|---|
| Other names
Zinc protoporphyrin IX | |
| Identifiers | |
| 15442-64-5 | |
| ChEBI | CHEBI:28783 |
| ECHA InfoCard | 100.035.853 |
| KEGG | C03184 |
| MeSH | zinc+protoporphyrin |
| PubChem | 27287 |
| Properties | |
| C34H32N4O4Zn | |
| Molar mass | 626.032 g/mol |
| Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |
| | |
| Infobox references | |
Zinc protoporphyrin (ZPP) is a compound found in red blood cells when heme production is inhibited by lead and/or by lack of iron. [1] Instead of incorporating a ferrous ion, to form heme, protoporphyrin IX, the immediate precursor of heme, incorporates a zinc ion, forming ZPP. The reaction to insert a ferrous ion into protoporphyrin IX is catalyzed by the enzyme ferrochelatase.
Clinical utility
Measurement of zinc protoporphyrin in red cells has been used as a screening test for lead poisoning.[2][3] and for iron deficiency.[4] There are a number of specific clinical situations in which this measurement has been found to be useful.[1]
Zinc protoporphyrin levels can be elevated as the result of a number of conditions, for instance:[2]
- lead poisoning
- iron deficiency
- sickle cell anemia
- sideroblastic anemia
- anemia of chronic disease
- vanadium exposure
- erythropoietic protoporphyria[5]
- Varying types of cancer
The virtue of elevated ZPP testing as a screen is that all of these conditions can be considered worth discovering.
The fluorescent properties of ZPP in intact red cells allows the ZPP/heme molar ratio to be measured quickly, at low cost, and in a small sample volume.[6]
More recently, ZnPP is finding a new use as a drug in combined cancer therapies.
History
Porphyrin compounds containing zinc have been known since the 1930s.[1] They became of more than academic interest with the discovery, in 1974,[7] that ZPP was the major non-heme porphyrin formed in red cells as the result of lead poisoning or iron deficiency.
It was already known at this time that non-heme Protoporphyrin IX levels were elevated in these conditions, but prior investigators had used acidic extraction methods in their assays that converted ZPP to unbound Protoporphyrin IX.[8]
The early literature is sometimes confusing, and results are hard to compare without detailed examination of the measurement methods and the conversion factors used to report the results.[9] Reports may refer to Free Erythrocyte Protoporphyrin (FEP) or Erythrocyte Protoporphyrin (EP or EPP). ZPP is also abbreviated ZP and ZnPP. Current practice is tending to measure and report the molar ratio of ZPP to Heme (μmole/mole).[1][4]
Zinc Protoporphyrin for Cancer Therapy
ZnPP is finding a new use in cancer therapies. Research into the field of nanotechnology is finding a use for many compounds which show different and often more favorable properties at the nanoscale. ZnPP is one such[10] compound that can effectively aid in the treatment of multiple types of cancer in laboratory experiments. The clinical application of the nanomaterial ZnPP will only come through continued research and more definitive results.[11]
The chemical group that ZnPP belongs to is similar to free heme which is a natural substrate of heme oxygenase.[12] ZnPP is known as a competitive inhibitor of heme oxygenase.[12] Heme oxygenase is a cytoprotective enzyme that copes with oxidative stress on a cell and shows higher expression in cancerous tissues.[13] ZnPP suppression of heme oxygenase reduces cell viability of cancer cells and increases cytotoxicity in cancer cells.[13] ZnPP works in combination with anticancer drugs to increase cytotoxicity greatly in some cases; results in one study have shown a five-fold increase in treatment efficacy.[14] ZnPP has been shown to have a major role in inhibiting tumor growth especially solid tumors.[14] Tumors from brain cancer, colon cancer, prostate cancer, renal cell cancer, oral squamous cell cancer, and leukemia all show a susceptibility to ZnPP due to increase expression of heme oxygenase.[14] The inhibition of heme oxygenase leads to an increase of reactive oxidative species in the cell which sensitizes the cells to chemotherapeutic agents.[10] Increased reactive oxidative species can cause apoptosis in cancer cells and reduce drug resistance when exposed to ZnPP due to loss of the heme oxygenase coping mechanism.[14] The combination of these two therapies is highly effective in treating cancer in experiments thus far, and is a possible new method for overcoming drug resistance. The reduced coping ability of tissues treated with ZnPP also increases radiosensitivity.[15] Cells treated with ZnPP and radiation as opposed to simply one of the two are less viable and more likely to stay in G1 phase of the cell cycle, rather than progress to the G2 phase.[15] ZnPP and radiation combination therapy shows more apoptosis than the same amount of radiation displaying that ZnPP puts stress on cancerous tissue.[15] ZnPP have been injected in a number of trials on solid tumors, but can be utilized more broadly when effectively delivered to cancer cells and not healthy cells.[10] A targeted delivery system is need to fully exploit the uses of ZnPP as a therapeutic agent and heme oxygenase inhibitor due to the potential side effects of free ZnPP on healthy tissue.[10] Reducing the anti-oxidant capability of healthy cells can reduce effects that would have been favorable.[10] However ZnPP have been encapsulated in nanoparticles with specialized coating for drug delivery inside the body.[10] ZnPP did not show any reduce inhibitory potential on heme oxygenase when loaded into nanoparticles.[10] Similarly ZnPP loaded into nanoparticles has a higher cytotoxicity than free ZnPP after two days due to a more favorable release rate as well as better biodistribution and internalization.[10] The possible negative effects on major organs were not seen and blood distribution is more desirable in ZnPP loaded nanoparticles than free ZnPP.[10] The specific inhibition of heme oxygenase using nanoparticles with encapsulated ZnPP reduces side effects and is likely the future method of administering ZnPP treatment.[10]
References
- 1 2 3 4 Labbé RF, Vreman HJ, Stevenson DK (December 1999). "Zinc protoporphyrin: A metabolite with a mission". Clinical Chemistry. 45 (12): 2060–72. PMID 10585337.
- 1 2 Martin CJ, Werntz CL, Ducatman AM (December 2004). "The interpretation of zinc protoporphyrin changes in lead intoxication: a case report and review of the literature". Occupational Medicine. 54 (8): 587–91. doi:10.1093/occmed/kqh123. PMID 15576877.
- ↑ Verschoor M, Herber R, Zielhuis R, Wibowo A (1987). "Zinc protoporphyrin as an indicator of lead exposure: precision of zinc protoporphyrin measurements". International Archives of Occupational and Environmental Health. 59 (6): 613–21. doi:10.1007/BF00377923. PMID 3679557.
- 1 2 Crowell R, Ferris AM, Wood RJ, Joyce P, Slivka H (July 2006). "Comparative effectiveness of zinc protoporphyrin and hemoglobin concentrations in identifying iron deficiency in a group of low-income, preschool-aged children: practical implications of recent illness". Pediatrics. 118 (1): 224–32. doi:10.1542/peds.2006-0156. PMID 16818569.
- ↑ http://beaunet.beaumont.edu/portal/pls/portal/lab.lab_pkg.lab_test_info_content?xid=862
- ↑ Blumberg WE, Eisinger J, Lamola AA, Zuckerman DM (February 1977). "The hematofluorometer". Clinical Chemistry. 23 (2 PT. 1): 270–4. PMID 832391.
- ↑ Lamola AA, Yamane T (December 1974). "Zinc protoporphyrin in the erythrocytes of patients with lead intoxication and iron deficiency anemia". Science. 186 (4167): 936–8. doi:10.1126/science.186.4167.936. PMID 4469690.
- ↑ Piomelli S (June 1973). "A micromethod for free erythrocyte porphyrins: the FEP test". The Journal of Laboratory and Clinical Medicine. 81 (6): 932–40. PMID 4710372.
- ↑ Some reports, for instance, measured the ZPP/Heme molar ratio (μmole ZPP per mole of heme), but reported this as the weight concentration (μg of EP per deciliter of packed red cells, or μg of EP per g hemoglobin at an assumed hematocrit of 35), and sometimes without easy access to the assumptions used in the conversion.
- 1 2 3 4 5 6 7 8 9 10 Kongpetch, S., Kukongviriyapan, V., Prawan, A., Senggunprai, L., Kukongviriyapan, U., & Buranrat, B. Crucial role of heme oxygenase-1 on the sensitivity of cholangiocarcinoma cells to chemotherapeutic agents. PLoS. One 2012, 7(4)
- ↑ Rouhani, H., Sepehri, N., Montazeri, H., Khoshayand, M. R., Ghahremani, M. H., Ostad, S. N., Dinarvand, R. Zinc protoporphyrin polymeric nanoparticles: Potent heme oxygenase inhibitor for cancer therapy. Pharm. Res. 2014, 31 (8), 2124-39.
- 1 2 Wang, S., Hannafon, B. N., Lind, S. E., & Ding, W. Zinc protoporphyrin suppresses beta]-catenin protein expression in human cancer cells: The potential involvement of lysosome-mediated degradation. PLoS. One 2015, 10(5)
- 1 2 Kang, K. A., Maeng, Y. H., Zhang, R., Yang, Y. R., Piao, M. J., Kim, K. C., Hyun, J. W.. Involvement of heme oxygenase-1 in korean colon cancer. Tumor Biol. 2012, 33(4), 1031-8
- 1 2 3 4 Yin, H., Fang, J., Liao, L., Maeda, H., & Su, Q. Upregulation of heme oxygenase-1 in colorectal cancer patients with increased circulation carbon monoxide levels, potentially affects chemotherapeutic sensitivity. BMC Cancer 2014, 14, 436.
- 1 2 3 Zhang, W., Qiao, T., & Zha, L. Inhibition of heme oxygenase-1 enhances the radiosensitivity in human nonsmall cell lung cancer A549 cells. Cancer Biother. Radiopharm. 2011, 26(5), 639-45.