Central core disease
| Central Core Disease Central core myopathy | |
|---|---|
.jpg) | |
| Histopathologic appearance of typical central core disease: NADH-TR, transverse section from the rectus femoris. Marked predominance of dark staining, high oxidative type 1 fibres with cores affecting the majority of fibres. Cores are typically well demarcated and centrally located (→), but may occasionally be multiple and of eccentric location. | |
| Classification and external resources | |
| Specialty | neurology |
| ICD-10 | G71.2 |
| ICD-9-CM | 359.0 |
| OMIM | 117000 |
| eMedicine | neuro/76 |
| MeSH | D020512 |
| GeneReviews | |
Central core disease (CCD), also known as central core myopathy, is an autosomal dominant[1] congenital myopathy (inborn muscle disorder). It was first described by Shy and Magee in 1956.[2][3] It is characterized by the appearance of the myofibril under the microscope.[4]
Signs and symptoms
The symptoms of CCD are variable, but usually involve hypotonia (decreased muscle tone) at birth, mild delay in child development (highly variable between cases), weakness of the facial muscles, and skeletal malformations such as scoliosis and hip dislocation.[2]
Symptoms may be present at birth or may appear at any stage of life. There appears to be a growing number of people who do not become symptomatic until adulthood to middle age. While generally not progressive, again there appears to be a growing number of people who do experience a slow clinically significant progression of symptomatology. These cases may hypothetically be due to the large number of gene mutations of ryanodine receptor malfunction, and with continued research may in fact be found to be clinical variants.
Diagnosis
The diagnosis is made on the combination of typical symptoms and the appearance on biopsy (tissue sample) from muscle. The name derives from the typical appearance of the biopsy on light microscopy, where the muscle cells have cores that are devoid of mitochondria and specific enzymes.[2]
Respiratory insufficiency develops in a small proportion of cases. Creatine kinase and electromyography (EMG) tend to be normal.[2]
Pathophysiology
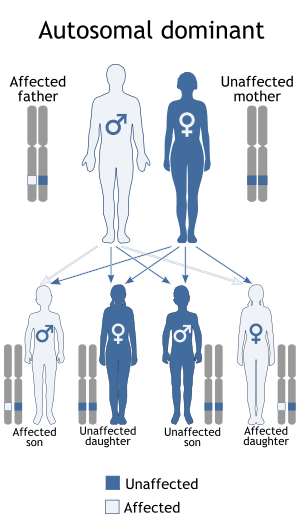
Central core disease is inherited in an autosomal dominant fashion. Most cases have demonstrable mutations in the ryanodine receptor type 1 (RYR1) gene,[1] which are often de novo (newly developed). People with CCD are at risk for malignant hyperthermia (MH) when receiving general anesthesia.[2]
Treatment
There is no specific treatment but triggering anesthetics are avoided and relatives are screened for RYR1 mutations as these may make them susceptible to MH.[2]
References
- 1 2 Robinson, Rl; Brooks, C; Brown, Sl; Ellis, Fr; Halsall, Pj; Quinnell, Rj; Shaw, Ma; Hopkins, Pm (August 2002). "RYR1 mutations causing central core disease are associated with more severe malignant hyperthermia in vitro contracture test phenotypes". Human Mutation. 20 (2): 88–97. doi:10.1002/humu.10098. PMID 12124989.
- 1 2 3 4 5 6 Quinlivan RM, Muller CR, Davis M, et al. (2003). "Central core disease: clinical, pathological, and genetic features". Arch. Dis. Child. 88 (12): 1051–5. doi:10.1136/adc.88.12.1051. PMC 1719384
 . PMID 14670767.
. PMID 14670767. - ↑ Magee KR, Shy GM (1956). "A new congenital non-progressive myopathy". Brain. 79 (4): 610–21. doi:10.1093/brain/79.4.610. PMID 13396066.
- ↑ "central core disease" at Dorland's Medical Dictionary