Decompression practice

The practice of decompression by divers comprises the planning and monitoring of the profile indicated by the algorithms or tables of the chosen decompression model, to allow asymptomatic and harmless release of excess inert gases dissolved in the tissues as a result of breathing at ambient pressures greater than surface atmospheric pressure, the equipment available and appropriate to the circumstances of the dive, and the procedures authorized for the equipment and profile to be used. There is a large range of options in all of these aspects.
Decompression may be continuous or staged, where the ascent is interrupted by stops at regular depth intervals, but the entire ascent is part of the decompression, and ascent rate can be critical to harmless elimination of inert gas. What is commonly known as no-decompression diving, or more accurately no-stop decompression, relies on limiting ascent rate for avoidance of excessive bubble formation. Staged decompression may include deep stops depending on the theoretical model used for calculating the ascent schedule. Omission of decompression theoretically required for a dive profile exposes the diver to significantly higher risk of symptomatic decompression sickness, and in severe cases, serious injury or death. The risk is related to the severity of exposure and the level of supersaturation of tissues in the diver. Procedures for emergency management of omitted decompression and symptomatic decompression sickness have been published. These procedures are generally effective, but vary in effectiveness from case to case.
The procedures used for decompression depend on the mode of diving, the available equipment, the site and environment, and the actual dive profile. Standardized procedures have been developed which provide an acceptable level of risk in the circumstances for which they are appropriate. Different sets of procedures are used by commercial, military, scientific and recreational divers, though there is considerable overlap where similar equipment is used, and some concepts are common to all decompression procedures.
Decompression
Decompression in the context of diving derives from the reduction in ambient pressure experienced by the diver during the ascent at the end of a dive or hyperbaric exposure and refers to both the reduction in pressure and the process of allowing dissolved inert gases to be eliminated from the tissues during this reduction in pressure. When a diver descends in the water column the ambient pressure rises. Breathing gas is supplied at the same pressure as the surrounding water, and some of this gas dissolves into the diver's blood and other fluids. Inert gas continues to be taken up until the gas dissolved in the diver is in a state of equilibrium with the breathing gas in the diver's lungs, (see: "Saturation diving"), or the diver moves up in the water column and reduces the ambient pressure of the breathing gas until the inert gases dissolved in the tissues are at a higher concentration than the equilibrium state, and start diffusing out again. Dissolved inert gases such as nitrogen or helium can form bubbles in the blood and tissues of the diver if the partial pressures of the dissolved gases in the diver gets too high above the ambient pressure. These bubbles and products of injury caused by the bubbles can cause damage to tissues known as decompression sickness, or "the bends". The immediate goal of controlled decompression is to avoid development of symptoms of bubble formation in the tissues of the diver, and the long-term goal is to also avoid complications due to sub-clinical decompression injury.[1][2][3]
Common procedures
The descent, bottom time and ascent are sectors common to all dives and hyperbaric exposures.
Descent rate
Descent rate is generally allowed for in decompression planning by assuming a maximum descent rate specified in the instructions for the use of the tables, but it is not critical.[4] Descent slower than the nominal rate reduces useful bottom time, but has no other adverse effect. Descent faster than the specified maximum will expose the diver to greater ingassing rate earlier in the dive, and the bottom time must be reduced accordingly. In the case of real time monitoring by dive computer, descent rate is not specified, as the consequences are automatically accounted for by the programmed algorithm.[5]
Bottom time
Bottom time is the time spent at depth before starting the ascent.[6] Bottom time used for decompression planning may be defined differently depending on the tables or algorithm used. It may include descent time, but not in all cases. It is important to check how bottom time is defined for the tables before they are used. For example, tables using Bühlmann's algorithm define bottom time as the elapsed time between leaving the surface and the start of the final ascent at 10 metres per minute, and if the ascent rate is slower, then the whole of the ascent time needs to be considered part of the bottom time for the algorithm to remain safe.[2]
Ascent rate
The ascent is an important part of the process of decompression, as this is the time when reduction of ambient pressure occurs, and it is of critical importance to safe decompression that the ascent rate is compatible with safe elimination of inert gas from the diver's tissues. Ascent rate must be limited to prevent supersaturation of tissues to the extent that unacceptable bubble development occurs. This is usually done by specifying a maximum ascent rate compatible with the decompression model chosen. This will be specified in the decompression tables or the user manual for the decompression software or personal decompression computer.[7] The instructions will usually include contingency procedures for deviation from the specified rate, both for delays and exceeding the recommended rate. Failure to comply with these specifications will generally increase the risk of decompression sickness.
Typically maximum ascent rates are in the order of 10 metres (33 ft) per minute for dives deeper than 6 metres (20 ft).[4] Some dive computers have variable maximum ascent rates, depending on depth. Ascent rates slower than the recommended standard for the algorithm will generally be treated by a computer as part of a multilevel dive profile and the decompression requirement adjusted accordingly. Faster ascent rates will elicit a warning and additional decompression stop time to compensate.[5]
No decompression dives
A "no decompression", or "no stop" dive is a dive that needs no decompression stops during the ascent according to the chosen algorithm or tables,[8] and relies on a controlled ascent rate for the elimination of excess inert gases. In effect, the diver is doing continuous decompression during the ascent.[7]
Safety stop
As a precaution against any unnoticed dive computer malfunction, diver error or physiological predisposition to decompression sickness, many divers do an extra "safety stop" in addition to those prescribed by their dive computer or tables.[9] A safety stop is typically 1 to 5 minutes at 3 to 6 metres (10 to 20 ft). They are usually done during no-stop dives and may be added to the obligatory decompression on staged dives. Many dive computers indicate a recommended safety stop as standard procedure for dives beyond specific limits of depth and time. The Goldman decompression model predicts a significant risk reduction following a safety stop on a low-risk dive[10]
No decompression limit
The no decompression limit (NDL) or no stop time, is the interval that a diver may theoretically spend at a given depth without having to perform decompression stops.[11] The NDL helps divers plan dives so that they can stay at a given depth and ascend without stopping while avoiding unacceptable risk of decompression sickness.
The NDL is a theoretical time obtained by calculating inert gas uptake and release in the body, using a model such as the Bühlmann decompression algorithm.[12] Although the science of calculating these limits has been refined over the last century, there is still much that is unknown about how inert gases enter and leave the human body. In addition, every individual's body is unique and may absorb and release inert gases at different rates. For this reason, dive tables typically have a degree of safety built into their recommendations. Divers can and do suffer decompression sickness while remaining inside NDLs, though the incidence is very low.[13] Each NDL for a range of depths is printed on dive tables in a grid that can be used to plan dives.[14] There are many different tables available as well as software programs and calculators, which will calculate no decompression limits. Most personal decompression computers (dive computers) will indicate a remaining no decompression limit at the current depth during a dive. The displayed interval is continuously revised to take into account changes of depth as well as elapsed time.[15]
Continuous decompression
Continuous decompression is decompression without stops. Instead of a fairly rapid ascent rate to the first stop, followed by a period at static depth during the stop, the ascent is slower, but without officially stopping. In theory this is the optimum decompression profile. In practice this is very difficult to do manually, and it may be necessary to stop the ascent occasionally to get back on schedule, but these stops are not part of the schedule, they are corrections. For example, USN treatment table 5, referring to treatment in a decompression chamber for type 1 decompression sickness, states "Descent rate - 20 ft/min. Ascent rate - Not to exceed 1 ft/min. Do not compensate for slower ascent rates. Compensate for faster rates by halting the ascent."[16]
To further complicate the practice, the ascent rate may vary with the depth, and is typically faster at greater depth and reduces as the depth gets shallower. In practice a continuous decompression profile may be approximated by ascent in steps as small as the chamber pressure gauge will resolve, and timed to follow the theoretical profile as closely as conveniently practicable. For example, USN treatment table 7 (which may be used if decompression sickness has reoccurred during initial treatment in the compression chamber) states "Decompress with stops every 2 feet for times shown in profile below." The profile shows an ascent rate of 2 fsw every 40 min from 60 fsw (feet of sea water) to 40 fsw, followed by 2 ft every hour from 40 fsw to 20 fsw and 2 ft every two hours from 20 fsw to 4 fsw.[16]
Staged decompression

Decompression which follows the procedure of relatively fast ascent interrupted by periods at constant depth is known as staged decompression. The ascent rate and the depth and duration of the stops are integral parts of the decompression process. The advantage of staged decompression is that it is far easier to monitor and control than continuous decompression.[12][17]
Decompression stops
A decompression stop is a period a diver must spend at a relatively shallow constant depth during ascent after a dive to safely eliminate absorbed inert gases from the body tissues to avoid decompression sickness. The practice of making decompression stops is called staged decompression,[12][17] as opposed to continuous decompression.[18][19]
The diver identifies the requirement for decompression stops, and if they are needed, the depths and durations of the stops, by using decompression tables,[16] software planning tools or a dive computer.
The ascent is made at the recommended rate until the diver reaches the depth of the first stop. The diver then maintains the specified stop depth for the specified period, before ascending to the next stop depth at the recommended rate, and follows the same procedure again. This is repeated until all required decompression has been completed and the diver reaches the surface.[12][20]
Once on the surface the diver will continue to eliminate inert gas until the concentrations have returned to normal surface saturation, which can take several hours, and is considered in some models to be effectively complete after 12 hours,[20] and by others to take up to, or even more than 24 hours.[12]
The depth and duration of each stop is calculated to reduce the inert gas excess in the most critical tissues to a concentration which will allow further ascent without unacceptable risk. Consequently, if there is not much dissolved gas, the stops will be shorter and shallower than if there is a high concentration. The length of the stops is also strongly influenced by which tissue compartments are assessed as highly saturated. High concentrations in slow tissues will indicate longer stops than similar concentrations in fast tissues.[12][20]
Shorter and shallower decompression dives may only need one single short shallow decompression stop, for example 5 minutes at 3 metres (10 ft). Longer and deeper dives often need a series of decompression stops, each stop being longer but shallower than the previous stop.[20]
Deep stops
A deep stop was originally an extra stop introduced by divers during ascent, at a greater depth than the deepest stop required by their computer algorithm or tables. This practice is based on empirical observations by technical divers such as Richard Pyle, who found that they were less fatigued if the made some additional stops for short periods at depths considerably deeper than those calculated with the currently published decompression algorithms. More recently computer algorithms that are claimed to use deep stops have become available, but these algorithms and the practice of deep stops have not been adequately validated.[21] Deep stops are likely to be made at depths where ingassing continues for some slow tissues, so the addition of deep stops of any kind can only be included in the dive profile when the decompression schedule has been computed to include them, so that such ingassing of slower tissues can be taken into account.[22] Nevertheless, deep stops may be added on a dive that relies on a personal dive computer with real-time computation, as the PDC will track the effect of the stop on its decompression schedule.[23] Deep stops are otherwise similar to any other staged decompression, but are unlikely to use a dedicated decompression gas, as they are usually not more than two to three minutes long.[24]
A study by Divers Alert Network in 2004 suggests that addition of a deep (c. 15 m) as well as a shallow (c. 6 m) safety stop to a theoretically no-stop ascent will significantly reduce decompression stress indicated by precordial doppler detected bubble (PDDB) levels. The authors associate this with gas exchange in fast tissues such as the spinal cord and consider that an additional deep safety stop may reduce the risk of spinal cord decompression sickness in recreational diving.[25] A follow-up study found that the optimum duration for the deep safety stop under the experimental conditions was 2.5 minutes, with a shallow safety stop of 3 to 5 minutes. Longer safety stops at either depth did not further reduce PDDB.[24]
In contrast, experimental work comparing the effect of deep stops observed a significant decrease in vascular bubbles following a deep stop after longer shallower dives, and an increase in bubble formation after the deep stop on shorter deeper dives, which is not predicted by the existing bubble model.[26]
A controlled comparative study by the Navy Experimental Diving Unit in the NEDU Ocean Simulation Facility wet-pot comparing the VVAL18 Thalmann Algorithm with a deep stop profile suggests that the deep stops schedule had a greater risk of DCS than the matched (same total stop time) conventional schedule. The proposed explanation was that slower gas washout or continued gas uptake offset benefits of reduced bubble growth at deep stops.[27][28]
Profile determined intermediate stops
PDISs are intermediate stops at a depth above the depth at which the leading compartment for the decompression calculation switches from ongassing to offgassing and below the depth of the first obligatory decompression stop, (or the surface, on a no-decompression dive). The ambient pressure at that depth is low enough to ensure that the tissues are mostly offgassing inert gas, although under a very small pressure gradient. This combination is expected to inhibit bubble growth. The leading compartment is generally not the fastest compartment except in very short dives, for which this model does not require an intermediate stop.[22]
The 8 compartment Bühlmann - based UWATEC ZH-L8 ADT MB PMG decompression model in the Scubapro Galileo dive computer processes the dive profile and suggests an intermediate 2-minute stop that is a function of the tissue nitrogen loading at that time, taking into account the accumulated nitrogen from previous dives.[22] Within the Haldanian logic of the model, at least three compartments are offgassing at the prescribed depth - the 5 and 10 minute half time compartments under a relatively high pressure gradient. Therefore, for decompression dives, the existing obligation is not increased during the stop.[29]
A PDIS is not a mandatory stop, nor is it considered a substitute for the more important shallow safety stop on a no-stop dive. Switching breathing gas mix during the ascent will influence the depth of the stop.[22]
The PDIS concept was introduced by Sergio Angelini.[29][30]
Decompression schedule
A decompression schedule is a specified ascent rate and series of increasingly shallower decompression stops—often for increasing amounts of time—that a diver performs to outgas inert gases from their body during ascent to the surface to reduce the risk of decompression sickness. In a decompression dive, the decompression phase may make up a large part of the time spent underwater (in many cases it is longer than the actual time spent at depth).[16]
The depth and duration of each stop is dependent on many factors, primarily the profile of depth and time of the dive, but also the breathing gas mix, the interval since the previous dive and the altitude of the dive site.[16] The diver obtains the depth and duration of each stop from a dive computer, decompression tables or dive planning computer software. A technical scuba diver will typically prepare more than one decompression schedule to plan for contingencies such as going deeper than planned or spending longer at depth than planned.[31] Recreational divers often rely on a personal dive computer to allow them to avoid obligatory decompression, while allowing considerable flexibility of dive profile. A surface supplied diver will normally have a diving supervisor at the control point who monitors the dive profile and can adjust the schedule to suit any contingencies as they occur.[16]
Missed stops
A diver missing a required decompression stop increases the risk of developing decompression sickness. The risk is related to the depth and duration of the missed stops. The usual causes for missing stops are: not having enough breathing gas to complete the stops, or accidentally losing control of buoyancy. An aim of most basic diver training is to prevent these two faults. There are also less predictable causes of missing decompression stops. Diving suit failure in cold water may force the diver to choose between hypothermia and decompression sickness. Diver injury or marine animal attack may also limit the duration of stops the diver is willing to carry out.[32]
A procedure for dealing with omitted decompression stops is described in the US Navy Diving Manual. In principle the procedure allows a diver who is not yet presenting symptoms of decompression sickness, to go back down and complete the omitted decompression, with some extra added to deal with the bubbles which are assumed to have formed during the period where the decompression ceiling was violated. Divers who become symptomatic before they can be returned to depth are treated for decompression sickness, and do not attempt the omitted decompression procedure as the risk is considered unacceptable under normal operational circumstances.[32]
If a decompression chamber is available, omitted decompression may be managed by chamber recompression to an appropriate pressure, and decompression following either a surface decompression schedule or a treatment table. If the diver develops symptoms in the chamber, treatment can be started without further delay.[32]
Accelerated decompression
Decompression can be accelerated by the use of breathing gases during ascent with lowered inert gas fractions (as a result of increased oxygen fraction). This will result in a greater diffusion gradient for a given ambient pressure, and consequently accelerated decompression for a relatively low risk of bubble formation.[33] Nitrox mixtures and oxygen are the most commonly used gases for this purpose, but oxygen rich trimix blends can also be used after a trimix dive, and oxygen rich heliox blends after a heliox dive, and these may reduce risk of isobaric counterdiffusion complications.[34] Doolette and Mitchell showed that when a switch is made to a gas with a different proportion of inert gas components, it is possible for an inert component previously absent, or present as a lower fraction, to in-gas faster than the other inert components are eliminated (inert gas counterdiffusion), sometimes resulting in raising the total tissue tension of inert gases in a tissue to exceed the ambient pressure sufficiently to cause bubble formation, even if the ambient pressure has not been reduced at the time of the gas switch. They conclude that "breathing-gas switches should be scheduled deep or shallow to avoid the period of maximum supersaturation resulting from decompression".[34]
Oxygen decompression
The use of pure oxygen for accelerated decompression is limited by oxygen toxicity. In open circuit scuba the upper limit for oxygen partial pressure is generally accepted as 1.6 bar,[35] equivalent to a depth of 6 msw (metres of sea water), but in-water and surface decompression at higher partial pressures is routinely used in surface supplied diving operation, both by the military and civilian contractors, as the consequences of CNS oxygen toxicity are considerably reduced when the diver has a secure breathing gas supply. US Navy tables (Revision 6) start in-water oxygen decompression at 30 fsw (9 msw), equivalent to a partial pressure of 1.9 bar, and chamber oxygen decompression at 50 fsw (15 msw), equivalent to 2.5 bar.[16]
Repetitive dives
Any dive which is started while the tissues retain residual inert gas in excess of the surface equilibrium condition is considered a repetitive dive. This means that the decompression required for the dive is influenced by the divers decompression history. Allowance must be made for inert gas preloading of the tissues which will result in them containing more dissolved gas than would have been the case if the diver had fully equilibrated before the dive. The diver will need to decompress longer to eliminate this increased gas loading.[6]
Surface interval
The surface interval (SI) or surface interval time (SIT) is the time spent by a diver at surface pressure after a dive during which inert gas which was still present at the end of the dive is further eliminated from the tissues.[6] This continues until the tissues are at equilibrium with the surface pressures. This may take several hours. In the case of the US Navy 1956 Air tables, it is considered complete after 12 hours,[16] The US Navy 2008 Air tables specify up to 16 hours for normal exposure.[36] but other algorithms may require more than 24 hours to assume full equilibrium.
Residual nitrogen time
For the planned depth of the repetitive dive, a bottom time can be calculated using the relevant algorithm which will provide an equivalent gas loading to the residual gas after the surface interval. This is called "residual nitrogen time" (RNT) when the gas is nitrogen. The RNT is added to the planned "actual bottom time" (ABT) to give an equivalent "total bottom time" (TBT) which is used to derive the appropriate decompression schedule for the planned dive.[6]
Equivalent residual times can be derived for other inert gases. These calculations are done automatically in personal diving computers, based on the diver's recent diving history, which is the reason why personal diving computers should not be shared by divers, and why a diver should not switch computers without a sufficient surface interval (more than 24 hours in most cases, up to 4 days, depending on the tissue model and recent diving history of the user).[37][38][39]
Residual inert gas can be computed for all modeled tissues, but repetitive group designations in decompression tables are generally based on only the one tissue, considered by the table designers to be the most limiting tissue for likely applications. In the case of the US Navy Air Tables (1956) this is the 120 minute tissue,[40] while the Bühlmann tables use the 80 minute tissue.[41]
Diving at altitude
The atmospheric pressure decreases with altitude, and this has an effect on the absolute pressure of the diving environment. The most important effect is that the diver must decompress to a lower surface pressure, and this requires longer decompression for the same dive profile.[42] A second effect is that a diver ascending to altitude, will be decompressing en route, and will have residual nitrogen until all tissues have equilibrated to the local pressures. This means that the diver should consider any dive done before equilibration as a repetitive dive, even if it is the first dive in several days.[43]
The US Navy diving manual provides repetitive group designations for listed altitude changes.[44] These will change over time with the surface interval according to the relevant table.[36]
Altitude corrections (Cross corrections) are described in the US Navy diving manual. This procedure is based on the assumption that the decompression model will produce equivalent predictions for the same pressure ratio. The "Sea Level Equivalent Depth" (SLED) for the planned dive depth, which is always deeper than the actual dive at altitude, is calculated[42] in inverse proportion to the ratio of surface pressure at the dive site to sea level atmospheric pressure.
- Sea level equivalent depth = Actual depth at altitude × Pressure at sea level ÷ Pressure at altitude
Decompression stop depths are also corrected, using the ratio of surface pressures, and will produce actual stop depths which are shallower than the sea level stop depths.
- Stop depth at altitude = Stop depth at sea level × Pressure at altitude ÷ Pressure at sea level
These values can be used with standard open circuit decompression tables, but are not applicable with constant oxygen partial pressure as provided by closed circuit rebreathers. Tables are used with the sea level equivalent depth and stops are done at the altitude stop depth.[45]
The decompression algorithms can be adjusted to compensate for altitude. This was first done by Bühlmann for deriving altitude corrected tables, and is now common on diving computers, where an altitude setting can be selected by the user.[12]
Flying and ascent to altitude after diving
Exposure to reduced atmospheric pressure during the period after a dive when the residual gas levels have not yet stabilized at atmospheric saturation levels can incur a risk of decompression sickness. Rules for safe ascent are based on extension of the decompression model calculations to the desired altitude, but are generally simplified to a few fixed periods for a range of exposures. For the extreme case of an exceptional exposure dive, the US Navy requires a surface interval of 48 hours before ascent to altitude. A surface interval of 24 hours for a Heliox decompression dive and 12 hours for Heliox no-decompression dive are also specified.[46] More detailed surface interval requirements based on the highest repetitive group designator obtained in the preceding 24‑hour period are given on the US Navy Diving Manual Table 9.6,[46] both for ascents to specified altitudes, and for commercial flights in aircraft nominally pressurized to 8000 ft.[47]
The first DAN flying after diving workshop in 1989 consensus guidelines recommended:[47]
- wait for 12 hours before flying after up to two hours of no-stop diving within the previous 48 hours;
- wait for 24 hours before flying after multi-day, unlimited no-stop diving;
- wait for 24–48 hours before flying after dives that required decompression stops;
- do not fly with DCS symptoms unless necessary to obtain hyperbaric treatment.
DAN later proposed a simpler 24-hour wait after any and all recreational diving, but there were objections on the grounds that such a long delay would result in lost business for island diving resorts and the risks of DCS when flying after diving were too low to warrant this blanket restraint.[47]
The DAN Flying after Diving workshop of 2002 made the following recommendations for flying after recreational diving:[47]
- a 12-hour surface interval for uncertified individuals who took part in a "resort" or introductory scuba experience;
- an 18-hour surface interval for certified divers who make an unlimited number of no-decompression air or nitrox dives over multiple days; and
- substantially longer than 18 hours for technical divers who make decompression dives or used helium breathing mixes, as no specific evidence concerning decompression or helium diving was available.
These recommendations apply to flying at an altitude greater than, or cabin pressure less than, an altitude equivalent of 2,000 feet (610 meters).[47]
NASA astronauts train underwater to simulate the weightlessness and occasionally need to fly afterwards at cabin altitudes not exceeding 10,000 feet (3,000 meters). Training dives use 46% Nitrox and can exceed six hours at a maximum depth of 40 ffw (12 mfw) for a maximum equivalent air depth (EAD) of 24 fsw (7 msw). NASA guidelines for EADs of 20–50 fsw (6–15 msw) with maximum dive durations of 100–400 minutes allow either air or oxygen to be breathed in the preflight surface intervals. Oxygen breathing during surface intervals reduces the time to fly by a factor of seven to nine times compared with air.[47] A study by another military organization, the Special Operations Command also indicated that preflight oxygen might be an effective means for reducing DCS risk.[47]
Some places, (for example, the Altiplano in Peru and Bolivia, or the plateau around Asmara (where the airport is) in Eritrea, and some mountain passes), are many thousand feet above sea level and travelling to such places after diving at lower altitude should be treated as flying at the equivalent altitude after diving.[47]
Specialised decompression procedures
Surface decompression

Surface decompression is a procedure in which some or all of the staged decompression obligation is done in a decompression chamber instead of in the water.[6] This reduces the time that the diver spends in the water, exposed to environmental hazards such as cold water or currents, which will enhance diver safety. The decompression in the chamber is more controlled, in a more comfortable environment, and oxygen can be used at greater partial pressure as there in no risk of drowning and a lower risk of oxygen toxicity convulsions. A further operational advantage is that once the divers are in the chamber, new divers can be supplied from the diving panel, and the operations can continue with less delay.[20]
A typical surface decompression procedure is described in the US Navy Diving Manual. If there is no in-water 40 ft stop required the diver is surfaced directly. Otherwise, all required decompression up to and including the 40 ft (12 m) stop is completed in-water. The diver is then surfaced and pressurised in a chamber to 50 fsw (15 msw) within 5 minutes of leaving 40 ft depth in the water. If this "surface interval" from 40 ft in the water to 50 fsw in the chamber exceeds 5 minutes, a penalty is incurred, as this indicates a higher risk of DCS symptoms developing, so longer decompression is required.[16]
In the case where the diver is successfully recompressed within the nominal interval, he will be decompressed according to the schedule in the air decompression tables for surface decompression, preferably on oxygen, which is used from 50 fsw (15 msw), a partial pressure of 2.5 bar. The duration of the 50 fsw stop is 15 minutes for the Revision 6 tables. The chamber is then decompressed to 40 fsw (12 msw) for the next stage of up to 4 periods on oxygen. A stop may also be done at 30 fsw (9 msw), for further periods on oxygen according to the schedule. Air breaks of 5 minutes are taken at the end of each 30 minutes of oxygen breathing.[16]
Surface decompression procedures have been described as "semi-controlled accidents".[48]
Data collected in the North Sea have shown that the overall incidence of decompression sickness for in-water and surface decompression is similar, but surface decompression tends to produce ten times more type II (neurological) DCS than in-water decompression. A possible explanation is that during the final stage of ascent, bubbles are produced that are stopped in the lung capillaries. During recompression of the diver in the deck chamber, the diameter of some of these bubbles is reduced sufficiently that they pass through the pulmonary capillaries and reach the systemic circulation on the arterial side, later lodging in systemic capillaries and causing neurological symptoms. The same scenario was proposed for type II DCS recorded after sawtooth profile diving or multiple repetitive diving.[49]
Dry bell decompression
"Dry", or "Closed" diving bells are pressure vessels for human occupation which can be deployed from the surface to transport divers to the underwater workplace at pressures greater than ambient. They are equalized to ambient pressure at the depth where the divers will get out and back in after the dive, and are then re-sealed for transport back to the surface, which also generally takes place with controlled internal pressure greater than ambient. During and/or after the recovery from depth, the divers may be decompressed in the same way as if they were in a decompression chamber, so in effect, the dry bell is a mobile decompression chamber. Another option, used in saturation diving, is to decompress to storage pressure (pressure in the habitat part of the saturation spread) and then transfer the divers to the saturation habitat under pressure (transfer under pressure – TUP), where they will stay until the next shift, or until decompressed at the end of the saturation period.[50]
Saturation decompression
Once all the tissue compartments have reached saturation for a given pressure and breathing mixture, continued exposure will not increase the gas loading of the tissues. From this point onwards the required decompression remains the same. If divers work and live at pressure for a long period, and are decompressed only at the end of the period, the risks associated with decompression are limited to this single exposure. This principle has led to the practice of saturation diving, and as there is only one decompression, and it is done in the relative safety and comfort of a saturation habitat, the decompression is done on a very conservative profile, minimising the risk of bubble formation, growth and the consequent injury to tissues. A consequence of these procedures is that saturation divers are more likely to suffer decompression sickness symptoms in the slowest tissues, whereas bounce divers are more likely to develop bubbles in faster tissues.[51]
Decompression from a saturation dive is a slow process. The rate of decompression typically ranges between 3 and 6 fsw (0.9 and 1.8 msw) per hour.[51]
| Depth range | Ascent rate |
|---|---|
| 1600 to 200 fsw | 6 fsw per hour |
| 200 to 100 fsw | 5 fsw per hour |
| 100 to 50 fsw | 4 fsw per hour |
| 50 to 0 fsw | 3 fsw per hour |
The US Navy Heliox saturation decompression rates require a partial pressure of oxygen to be maintained at between 0.44 and 0.48 atm when possible, but not to exceed 23% by volume, to restrict the risk of fire.[51] For practicality the decompression is done in increments of 1 fsw at a rate not exceeding 1 fsw per minute, followed by a stop, with the average complying with the table ascent rate. Decompression is done for 16 hours in 24, with the remaining 8 hours split into two rest periods. A further adaptation generally made to the schedule is to stop at 4 fsw for the time that is would theoretically take to complete the decompression at the specified rate, i.e. 80 minutes, and then complete the decompression to surface at 1 fsw per minute. This is done to avoid the possibility of losing the door seal at a low pressure differential and losing the last hour or so of slow decompression.[51]
The Norwegian saturation decompression tables are similar, but specifically do not allow decompression to start with an upward excursion. Partial pressure of oxygen is maintained between 0.4 and 0.5 bar, and a rest stop of 6 hours is specified each night starting at midnight.[52]
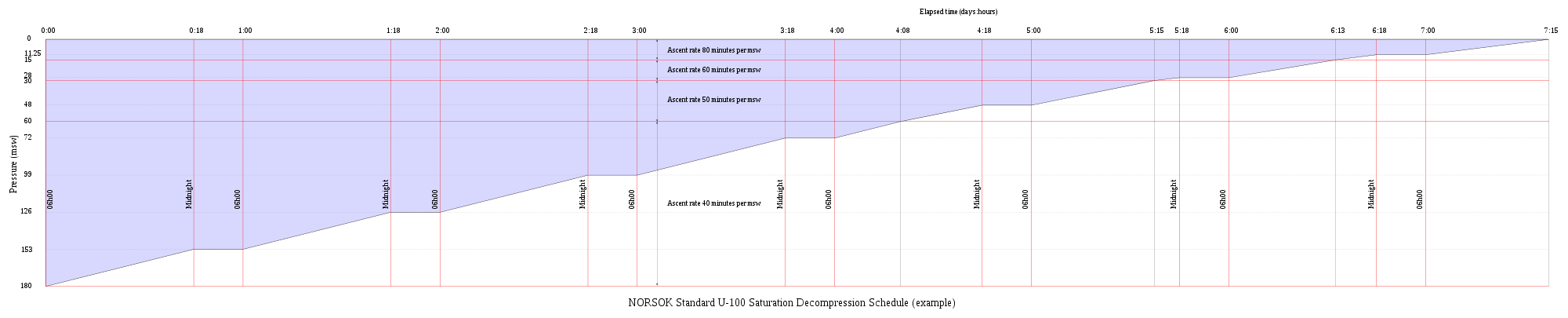
| Depth range | Ascent rate | Ascent rate |
|---|---|---|
| 180 to 60 msw | 40 minutes/msw | 27 msw/day |
| 60 to 30 msw | 50 minutes/msw | 21,6 msw/day |
| 30 to 15 msw | 60 minutes/msw | 18 msw/day |
| 15 to 0 msw | 80 minutes/msw | 13,5 msw/day |
Therapeutic decompression
Therapeutic decompression is a procedure for treating decompression sickness by recompressing the diver, thus reducing bubble size, and allowing the gas bubbles to re-dissolve, then decompressing slowly enough to avoid further formation or growth of bubbles, or eliminating the inert gases by breathing oxygen under pressure.[50]
Therapeutic decompression on air
Recompression on atmospheric air was shown to be an effective treatment for minor DCS symptoms by Keays in 1909.[53]
Historically, therapeutic decompression was done by recompressing the diver to the depth of relief of pain, or a bit deeper, maintaining that pressure for a while, so that bubbles could be re-dissolved, and performing a slow decompression back to the surface pressure. Later air tables were standardised to specific depths, followed by slow decompression. This procedure has been superseded almost entirely by hyperbaric oxygen treatment.[16][54][55][56]
Hyperbaric oxygen therapy
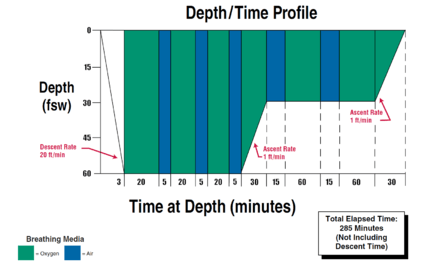
Evidence of the effectiveness of recompression therapy utilizing oxygen was first shown by Yarbrough and Behnke,[56] and has since become the standard of care for treatment of DCS.[57]
A typical hyperbaric oxygen treatment schedule is the US Navy Table 6, which provides for a standard treatment of 3 to 5 periods of 20 minutes of oxygen breathing at 60 fsw (18msw) followed by 2 to 4 periods of 60 minutes at 30 fsw (9 msw) before surfacing. Air breaks are taken between oxygen breathing to reduce the risk of oxygen toxicity.[16]
In water recompression
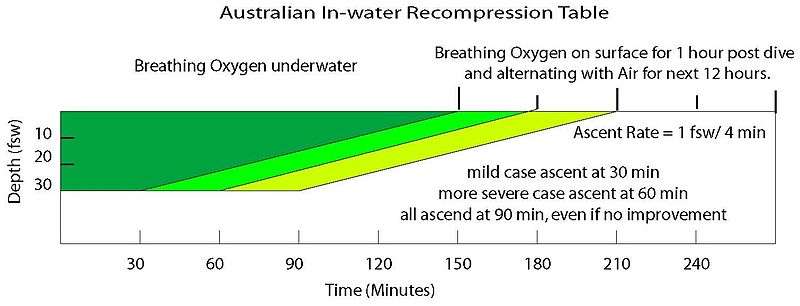
If a chamber is not available for recompression within a reasonable period, a riskier alternative is in-water recompression at the dive site.[58][59][60] In-water recompression (IWR) is the emergency treatment of decompression sickness (DCS) by sending the diver back underwater to allow the gas bubbles in the tissues, which are causing the symptoms, to resolve. It is a risky procedure that should only be used when it is not practicable to travel to the nearest recompression chamber in time to save the victim's life.[59][60]
The procedure is high risk as a diver suffering from DCS may become paralysed, unconscious or stop breathing whilst under water. Any one of these events may result in the diver drowning or further injury to the diver during a subsequent rescue to the surface. These risks can be mitigated to some extent by using a helmet or full-face mask with voice communications on the diver, and suspending the diver from the surface so that depth is positively controlled, and by having an in-water standby diver attend the diver undergoing the treatment at all times.[61]
The principle behind in water recompression treatment is the same as that behind the treatment of DCS in a recompression chamber[59][60]
Although in-water recompression is regarded as risky, and to be avoided, there is increasing evidence that technical divers who surface and demonstrate mild DCS symptoms may often get back into the water and breathe pure oxygen at a depth 20 feet (6.1 m) for a period to seek to alleviate the symptoms. This trend is noted in paragraph 3.6.5 of DAN's 2008 accident report.[62] The report also notes that whilst the reported incidents showed very little success, "[w]e must recognize that these calls were mostly because the attempted IWR failed. In case the IWR were successful, [the] diver would not have called to report the event. Thus we do not know how often IWR may have been used successfully."[62]
Historically, in-water recompression was the usual method of treating decompression sickness in remote areas. Procedures were often informal and based on operator experience, and used air as the breathing gas as it was all that was available. The divers generally used standard diving gear, which was relatively safe for this procedure, as the diver was at low risk of drowning if he lost consciousness.[63]
Decompression equipment
There are several types of equipment used to help divers carry out decompression. Some are used to plan and monitor the decompression and some mark the underwater position of the diver and act as a buoyancy control aid and position reference in low visibility or currents. Decompression may be shortened (or accelerated) by breathing an oxygen-rich "deco gas" such as a nitrox with 50% or more oxygen. The high partial pressure of oxygen in such decompression mixes create the effect of the oxygen window.[64] This decompression gas is often carried by scuba divers in side-slung cylinders. Cave divers who can only return by a single route, will often leave decompression gas cylinders attached to the guideline at the points where they will be used.[65] Surface supplied divers will have the composition of the breathing gas controlled at the gas panel.[66] Divers with long decompression obligations may be decompressed inside gas filled chambers in the water or at the surface.
Planning and monitoring decompression
Equipment for planning and monitoring decompression includes decompression tables, surface computer software and personal decompression computers. There is a wide range of choice:
- A decompression algorithm is used to calculate the decompression stops needed for a particular dive profile to reduce the risk of decompression sickness occurring after surfacing at the end of a dive. The algorithm can be used to generate decompression schedules for a particular dive profile, decompression tables for more general use, or be implemented in dive computer software.[5] Depending on the algorithm chosen the range of no-decompression limits at a given depth on the same gas can vary considerably. It is not possible to discriminate between "right" and "wrong" options, but it is considered correct to say that the risk of developing DCS is greater for the longer exposures and less for the shorter exposures for a given depth.[13]
- Dive tables or decompression tables are tabulated data, often in the form of printed cards or booklets, that allow divers to determine a decompression schedule for a given dive profile and breathing gas.[67] In some cases they may also specify an altitude range.[20] The choice of tables for professional diving use is generally made by the organization employing the divers, and for recreational training it is usually prescribed by the certifying agency, but for recreational purposes the diver is generally free to make use of any of the range of published tables, and for that matter, to modify them to suit himself or herself.[13]
- Decompression software is available for personal computers to model the decompression requirements of user specified dive profiles with different gas mixtures using a choive of decompression algorithms.[68][69][70][71] Schedules generated by decompression software represent a diver's specific dive plan and breathing gas mixtures. It is usual to generate a schedule for the planned profile and for the most likely contingency profiles.
- A personal dive computer is a small computer designed to be worn by a diver during a dive, with a pressure sensor and an electronic timer mounted in a waterproof and pressure resistant housing which has been programmed to model the inert gas loading of the diver's tissues in real time during a dive.[72] A display allows the diver to see critical data during the dive, including the maximum and current depth, duration of the dive, and decompression data including the remaining no decompression limit calculated in real time for the diver throughout the dive. The dive computer keeps track of residual gas loading for each tissue used in the algorithm.[73] Dive computers also provide a measure of safety for divers who accidentally dive a different profile to that originally planned. Most dive computers will provide the necessary decompression information for acceptably safe ascent in the event that the no-decompression limits are exceeded.[73] The use of computers to manage recreational dive decompression is becoming the standard and their use is also common in occupational scientific diving. Their value in surface supplied commercial diving is more restricted, but they can usefully serve as a dive profile recorder.[23]
Controlling depth and ascent rate


A critical aspect of successful decompression is that the depth and ascent rate of the diver must be monitored and sufficiently accurately controlled. Practical in-water decompression requires a reasonable tolerance for variation in depth and rate of ascent, but unless the decompression is being monitored in real time by a decompression computer, any deviations from the nominal profile will affect the risk. Several items of equipment are used to assist in facilitating accurate adherence to the planned profile, by allowing the diver to more easily control depth and ascent rate, or to transfer this control to specialist personnel at the surface.[74]
- A shot line is a rope between a float at the surface, and a sufficiently heavy weight holding the rope approximately vertical. The shot line float should be sufficiently buoyant to support the weight of all divers that are likely to be using it at the same time. Recreational divers are free to choose lesser buoyancy at their own risk. The shot weight should be sufficient to prevent a diver from lifting it from the bottom by over-inflation of the buoyancy compensator or dry suit, but not sufficient to sink the float if the slack on the line is all taken up. Various configurations of shot line are used to control the amount of slack.[75] The diver ascends along the shotline, and may use it purely as a visual reference, or can hold on to it to positively control depth, or can climb up it hand over hand. A Jonline may be used to fasten a diver to a shotline during a decompression stop.[75]
- A decompression trapeze is a device used in recreational diving and technical diving to make decompression stops more comfortable and more secure and provide the divers' surface cover with a visual reference for the divers' position.[75] It consists of a horizontal bar or bars suspended at the depth of intended decompression stops by buoys. The bars are of sufficient weight and the buoys of sufficient buoyancy that the trapeze will not easily change depth in turbulent water or if the divers experience buoyancy control problems.[75][76]
- A surface marker buoy (SMB) with a reel and line is often used by a dive leader to allow the boat to monitor progress of the dive group. This can provide the operator with a positive control of depth, by remaining slightly negative and using the buoyancy of the float to support this slight over-weighting. This allows the line to be kept under slight tension which reduces the risk of entanglement. The reel or spool used to store and roll up the line usually has slightly negative buoyancy, so that if released it will hang down and not float away.[77][78]
- A delayed or deployable surface marker buoy (DSMB) is a soft inflatable tube which is attached to a reel or spool line at one end, and is inflated by the diver under water and released to float to the surface, deploying the line as it ascends. This provides information to the surface that the diver is about to ascend, and where he is. This equipment is commonly used by recreational and technical divers, and requires a certain level of skill to operate safely. They are mostly used to signal the boat that the diver has started ascent or to indicate a problem in technical diving.[78][79][80]
- A diving stage, sometimes known as the basket, or diver launch and recovery system (LARS), is a platform on which one or two divers stand which is hoisted into the water, lowered to the workplace or the bottom, and then hoisted up again to return the diver to the surface and lift him out of the water. This equipment is almost exclusively used by surface supplied professional divers, as it requires fairly complex lifting equipment. A diving stage allows the surface team to conveniently manage a diver's decompression as it can be hoisted at a controlled rate and stopped at the correct depth for decompression stops, and allows the divers to rest during the ascent. It also allows the divers to be relatively safely and conveniently lifted out of the water and returned to the deck or quayside.[81][82]
- A wet bell, or open bell, is similar to a diving stage in concept, but has an air space, open to the water at the bottom in which the divers, or at least their heads, can shelter during ascent and descent.[49]
Providing gases to accelerate decompression

Reducing the partial pressure of the inert gas component of the breathing mixture will accelerate decompression as the concentration gradient will be greater for a given depth. This is usually achieved by increasing the partial pressure of oxygen in the breathing gas, as substituting a different inert gas may have counter-diffusion complications due to differing rates of diffusion, which can lead to a net gain in total dissolved gas tension in a tissue. This can lead to bubble formation and growth, with decompression sickness as a consequence. Partial pressure of oxygen is usually limited to 1.6 bar during in water decompression for scuba divers, but can be up to 1.9 bar in-water and 2.2 bar in the chamber when using the US Navy tables for surface decompression.[83]
- Stage cylinders are cylinders which are stored by scuba divers along the return route containing decompression and emergency gas. This is only practicable where the return route is known and marked by a guideline. Similar cylinders are carried by the divers when the route back is not secure. They are commonly mounted as sling cylinders, clipped to D-rings at the sides of the diver's harness.[84] The divers must avoid breathing oxygen enriched "deco gas" at excessive depths because of the high risk of oxygen toxicity. To prevent this happening, cylinders containing oxygen-rich gases must always be positively identifiable. One way of doing this is by marking them with their maximum operating depth as clearly as possible.[84]
- Surface supplied divers may be supplied with a gas mixture suitable for accelerated decompression by connecting a supply to the surface gas panel and providing it through the umbilical to the divers. This allows accelerated decompression, usually on oxygen, which can be used to a maximum depth of 30 ft (9 m).[83] Surface supplied heliox bounce divers will be provided with mixtures suitable for their current depth, and the mixture may be changed several times during descent and ascent from great depths.[85]
- Closed circuit rebreathers are usually controlled to provide a fairly constant partial pressure of oxygen during the dive (set point), and may be reset to a richer mix for decompression. The effect is to keep the partial pressure of inert gases as low as safely practicable throughout the dive. This minimizes the absorption of inert gas in the first place, and accelerates the elimination of the inert gases during ascent.[86]
Surface decompression

Specialised equipment is available to decompress a diver out of the water. This is almost exclusively used with surface supplied diving equipment:
- Deck decompression chambers are used for surface decompression, described in a previous section. Most deck decompression chambers are fitted with built in breathing systems (BIBS), which supply an alternative breathing gas to the occupants (usually oxygen), and discharge the exhaled gas outside the chamber, so the chamber gas is not excessively enriched by oxygen, which would cause an unacceptable fire hazard, and require frequent flushing with chamber gas (usually air).[87]

- A dry bell may be used for bounce dives to great depths, and then used as the decompression chamber during the ascent and later on board the support vessel. In this case it is not always necessary to transfer into a deck chamber, as the bell is quite capable of performing this function, though it would be relatively cramped, as a bell is usually as small as conveniently possible to minimize weight for deployment.[88]
- A Saturation System or Saturation spread typically comprises a living chamber, transfer chamber and submersible decompression chamber, which is commonly referred to in commercial diving as the diving bell and in military diving as the personnel transfer capsule,[89] PTC (Personnel Transfer Capsule) or SDC (Submersible Decompression Chamber).[90] The diving bell is the elevator or lift that transfers divers from the system to the work site and back. At the completion of work or a mission, the saturation diving team is decompressed gradually back to atmospheric pressure by the slow venting of system pressure, at rates of about of 15 metres (49 ft) to 30 metres (98 ft) per day, (schedules vary). Thus the process involves only one ascent, thereby mitigating the time-consuming and comparatively risky process of multiple decompressions normally associated with multiple non-saturation ("bounce diving") operations.[88]
- A hyperbaric lifeboat or hyperbaric rescue unit may be provided for emergency evacuation of saturation divers from a saturation system. This would be used if the platform is at immediate risk due to fire or sinking, and allows the divers under saturation to get clear of the immediate danger. The crew would normally start decompression as soon as possible after launching.[91]
Teaching of decompression practice
Basic decompression theory and use of decompression tables is part of the theory component of training for commercial divers,[92] and dive planning based on decompression tables, and the practice and field management of decompression is a significant part of the work of the diving supervisor.[16][93]
Recreational divers are trained in the theory and practice of decompression to the extent that the certifying agency specifies in the training standard for each certification. This may vary from a rudimentary overview sufficient to allow the diver to avoid decompression obligation for entry level divers, to competence in the use of several decompression algorithms by way of personal dive computers, decompression software, and tables for advanced technical divers.[31] The detailed understanding of decompression theory is not generally required of either commercial or recreational divers.
The practice of decompression techniques is another matter altogether. Recreational divers are expected not to do decompression dives by most certification organizations,[94][95] though CMAS and BSAC allow for short decompression dives in some levels of recreational divers.[96][97] Technical, commercial, military and scientific divers may all be expected to do decompression dives in the normal course of their sport or occupation, and are specifically trained in appropriate procedures and equipment relevant to their level of certification. A significant part of practical and theoretical training for these divers is on the practice of safe and effective decompression procedures and the selection and use of the appropriate equipment.[31][98][99]
See also
- Decompression (diving)
- Decompression sickness
- Decompression theory
- History of decompression research and development
References
- ↑ Staff (15 April 2008). "9-2, Theory of Decompression". U.S. Navy Diving Manual (R6 ed.). Naval sea systems command, US Navy.
- 1 2 James W. Miller, ed. (1979). "10.5 Decompression aspects of air diving". NOAA Diving Manual (2nd ed.). United States Department of Commerce.
- ↑ James W. Miller, ed. (1979). "2.2.3 Indirect effects of pressure". NOAA Diving Manual (2nd ed.). United States Department of Commerce.
- 1 2 Staff (15 April 2008). "9-6 General rules for the use of Air Decompression Tables". U.S. Navy Diving Manual (R6 ed.). Naval sea systems command, US Navy.
- 1 2 3 Huggins, KE (2012). "Dive Computer Considerations: How dive computers work". Proceedings of the Validation of Dive Computer Workshop convened by the Baromedical and Environmental Physiology Group of NTNU on August 24, 2011, at the 37th Annual Meeting of the European Underwater and Baromedical Society in Gdansk, Poland. NTNU and the Norwegian Labour Inspection Authority. Retrieved 6 March 2016.
- 1 2 3 4 5 Staff (15 April 2008). "9-3 Air Decompression definitions". U.S. Navy Diving Manual (R6 ed.). Naval sea systems command, US Navy.
- 1 2 Huggins 1992, chpt. 3 page 9
- ↑ Staff (15 April 2008). "9-3.12". U.S. Navy Diving Manual (R6 ed.). Naval sea systems command, US Navy.
- ↑ Uguccioni, DM (1984). Doppler Detection of Silent Venous Gas Emboli in Non-Decompression Diving Involving Safety Stops. Wilmington, NC: University of North Carolina at Wilmington. Retrieved 2008-04-25.
- ↑ Goldman, Saul; Goldman, Ethel (2014). "To stop or not to stop and why?" (PDF). Alert Diver. DAN South Africa. 6 (2): 34–37. ISSN 2071-7628. Retrieved 10 September 2014.
- ↑ Staff (15 April 2008). "9-3.11". U.S. Navy Diving Manual (R6 ed.). Naval sea systems command, US Navy.
- 1 2 3 4 5 6 7 Bühlmann Albert A. (1984). Decompression–Decompression Sickness. Berlin New York: Springer-Verlag. ISBN 0-387-13308-9.
- 1 2 3 Huggins 1992, Introduction page 1
- ↑ Staff (15 April 2008). "9-7". U.S. Navy Diving Manual (R6 ed.). Naval sea systems command, US Navy.
- ↑ Huggins, KE (2012). "Dive Computer Considerations". Proceedings of the Validation of Dive Computer Workshop. European Underwater and Baromedical Society. Retrieved 4 March 2016.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 US Navy Diving Manual Revision 6
- 1 2 Boycott, A. E.; G. C. C. Damant, J. S. Haldane. (1908). "The Prevention of Compressed-air Illness". J. Hygiene. 8 (3): 342–443. doi:10.1017/S0022172400003399. PMC 2167126
 . PMID 20474365. Retrieved 2008-08-06.
. PMID 20474365. Retrieved 2008-08-06. - ↑ Bert, P. (1943). "Barometric Pressure: researches in experimental physiology". Translated by: Hitchcock MA and Hitchcock FA. College Book Company; originally published 1878.
- ↑ Sport Diving, British Sub Aqua Club, ISBN 0-09-163831-3, page 110
- 1 2 3 4 5 6 US Navy Diving Manual Revision 6, chpt. 9 sect. 8 The air decompression table
- ↑ Denoble, Petar (Winter 2010). "Deep stops". Alert Diver. Diver Alert Network. Retrieved 3 August 2015.
- 1 2 3 4 Staff. "Diving with PDIS (Profile-Dependent Intermediate Stop)" (PDF). Dykkercentret website. Frederiksberg: Dykkercentret ApS. Retrieved 5 March 2016.
- 1 2 Azzopardi, E; Sayer, MDJ (2010). "A review of the technical specifications of 47 models of diving decompression computer". International Journal of the Society for Underwater Technology. Society for Underwater Technology. 29 (2): 63–70. doi:10.3723/ut.29.063. Retrieved 7 March 2016.
- 1 2 Bennett, PB; Marroni, A; Cronje, FJ; Cali-Corleo, R; Germonpre, P; Pieri, M; Bonuccelli, C; Leonardi, MG; Balestra, C (2007). "Effect of varying deep stop times and shallow stop times on precordial bubbles after dives to 25 msw (82 fsw).". Undersea & Hyperbaric Medicine : Journal of the Undersea and Hyperbaric Medical Society, Inc. Undersea and Hyperbaric Medical Society, Inc. Retrieved 5 March 2016.
- ↑ Marroni, A; Bennett, PB; Cronje, FJ; Balestra, C; Cali-Corleo, R; Germonpre, P; Pieri, M; Bonuccelli, C (2004). "Use of a deep (15m) and shallow (6m) stop following 25 meter no-decompression dives reduces decompression stress (as observed by doppler-detectable bubbles) when compared to either a direct ascent, or direct ascent with only a shallow stop.". Undersea and Hyperbaric Medical Society, Inc. Retrieved 5 March 2016.
- ↑ Gutvik, CR; Møllerløkken, A; Brubakk, AO (2007). "Difference in bubble formation using deep stops is dependent on length of bottom time; experimental findings and theoretical support.". Abstract of the Undersea and Hyperbaric Medical Society, Inc. Annual Scientific Meeting held June 14–16, 2007. Ritz-Carlton Kapalua Maui, Hawaii. Undersea and Hyperbaric Medical Society, Inc. Retrieved 5 March 2016.
- ↑ Gerth, WA; Gault, KA; Doolette, DJ (2007). "Empirical evaluation of the efficacy of deep stops in air decompression dives.". Abstract of the Undersea and Hyperbaric Medical Society, Inc. Annual Scientific Meeting held June 14–16, 2007. Ritz-Carlton Kapalua Maui, Hawaii. Undersea and Hyperbaric Medical Society, Inc. Retrieved 6 March 2016.
- ↑ Doolette, DJ; Gerth, WA; Gault, KA (2011). "Redistribution of decompression stop time from shallow to deep stops increases incidence of decompression sickness in air decompression dives". TA 04-12 NEDU TR 11-06. 1333 Isaac Hull Avenue, SE Washington Navy Yard D.C. 2037: Naval Sea Systems Command. Retrieved 6 March 2016.
- 1 2 Angelini, S (2008). "PDIS: Profile - Dependent Intermediate Stop.". Abstract of the Undersea & Hyperbaric Medical Society 2008 Annual Scientific Meeting June 26–28, 2008 Salt Lake City Marriott Downtown, Salt Lake City, Utah. Undersea & Hyperbaric Medical Society 2008. Retrieved 5 March 2016.
- ↑ Staff (2014). "PHYPODE People » Sergio Angelini, Ph.D". PHYPODE project website. PHYPODE project. Retrieved 5 March 2016.
- 1 2 3 Beresford, M.: CMAS-ISA Normoxic Trimix Manual
- ↑ Latson, Gary (December 2000). "Accelerated decompression using oxygen for submarine rescue - Summary report and operational guidance". Navy Experimental Diving Unit. Retrieved 3 March 2016.
- 1 2 Doolette, David J; Mitchell, Simon J (June 2003). "Biophysical basis for inner ear decompression sickness". Journal of Applied Physiology. 94 (6): 2145–50. doi:10.1152/japplphysiol.01090.2002 (inactive 2015-01-01). PMID 12562679. Retrieved 10 January 2010.
- ↑ Staff (2015). "Oxygen partial pressure". BSAC Safe Diving. British Sub-Aqua Club. p. 35. Retrieved 6 March 2016.
- ↑ Staff (2012). "Safety precautions" (PDF). Suunto D4i UserGuide. Suunto Oy. p. 8. Retrieved 6 March 2016.
- ↑ Staff (2006). "Safety" (PDF). Oceanic dive computer safety and reference manual. Doc No. 12-2262 r06. San Leandro, CA 94577: Oceanic USA. p. 14. Retrieved 6 March 2016.
- ↑ Staff. "Safety considerations" (PDF). Operating Manual: Uwatec Aladin Prime, Aladin Tec. Uwatec AG. p. 3. Retrieved 6 March 2016.
- ↑ Huggins 1992, chpt. 3 page 13
- ↑ Huggins 1992, chpt. 4 pages 2–3
- 1 2 3 4 5 6 7 8 Paul J. Sheffield, D. Richard D. Vann, (2002), Flying After Recreational Diving Workshop Proceedings, Divers Alert Network, Durham, North Carolina. http://archive.rubicon-foundation.org/xmlui/handle/123456789/5611 Accessed 2012-02-06
- ↑ Gorman, Des F (1989). "Decompression tables: their use and problems". South Pacific Underwater Medicine Society Journal. 19 (3): 111–113. Retrieved 2011-10-31.
- 1 2 Imbert, Jean Pierre (February 2006). Lang and Smith, eds. "Commercial Diving: 90m Operational Aspects" (PDF). Advanced Scientific Diving Workshop. Smithsonian Institution. Retrieved 2012-06-30.
- 1 2 3 4 5 Staff, US Navy (2006). "15". US Navy Diving Manual, 6th revision. United States: US Naval Sea Systems Command. Retrieved 2008-06-15.
- 1 2 Staff (April 2009). NORSOK Standard U-100 : Manned underwater operations (3 ed.). Lysaker , Norway: Standards Norway.
- ↑ Keays, FJ (1909). "Compressed air illness, with a report of 3,692 cases". Department of Medicine Publications of Cornell University Medical College 2: 1–55.
- ↑ Moon, RE (2000). "Recompression treatments should be to a pressure equivalent to 18 m depth. (Part 2 of 5 part Pro Con Debate)". South Pacific Underwater Medicine Society Journal. 30 (3). ISSN 0813-1988. OCLC 16986801. Retrieved 2008-06-08.
- ↑ Berghage, T. E.; J. Vorosmarti Jr; E. E. P. Barnard. (1978). "Recompression treatment tables used throughout the world by government and industry". US Naval Medical Research Center Technical Report. NMRI-78-16. Retrieved 2008-06-08.
- 1 2 Yarbrough, O. D.; Albert R. Behnke (1939). "The treatment of compressed air illness using oxygen". J Ind Hyg Toxicol. 21: 213–218. ISSN 0095-9030.
- ↑ Berghage, Thomas E; Vorosmarti Jr, James; Barnard, EEP (1978). "Recompression treatment tables used throughout the world by government and industry". US Naval Medical Research Center Technical Report NMRI-78-16. http://archive.rubicon-foundation.org/3414. Retrieved 25 May 2010.
- ↑ Edmonds, Carl (1998). "Underwater oxygen for treatment of decompression sickness: A review". South Pacific Underwater Medicine Society Journal. 25 (3). ISSN 0813-1988. OCLC 16986801. Retrieved 2011-10-31.
- 1 2 3 Pyle, Richard L.; Youngblood, David A (1995). "In-water Recompression as an emergency field treatment of decompression illness". AquaCorp. 11. Retrieved 2008-06-08.
- 1 2 3 Kay, E; M. P. Spencer (1999). In water recompression. 48th Undersea and Hyperbaric Medical Society Workshop. UHMS Publication Number RC103.C3. United States: Undersea and Hyperbaric Medical Society. p. 108. Retrieved 2008-06-08.
- 1 2 Vann, Richard D; Uguccioni, Donna M (eds). "Annual Diving Report:2008 edition" (PDF). Divers Alert Network. Retrieved 2009-09-01.
- ↑ LeMessurier and Hills. (1965) Decompression Sickness. A thermodynamic approach arising from a study on Torres Strait diving techniques. Hvalradets Skrifter, Nr. 48, 54–84.
- ↑ Van Liew, Hugh D; Bishop, B; Walder, P; Rahn, H (1965). "Effects of compression on composition and absorption of tissue gas pockets". Journal of Applied Physiology. 20 (5): 927–33. ISSN 0021-8987. OCLC 11603017. PMID 5837620.
- ↑ Staff (13 April 2010). "Using multiple cylinders". Sport Diver (online magazine). PADI. Retrieved 3 March 2016.
- ↑ Huggins 1992, chpt. 4 pages 1 - 18
- ↑ "Departure – Dive Planning and Decompression software". Diverssupport.com. Retrieved 2012-07-17.
- ↑ "DecoPlanner, decompression simulation software". Gue.com. Retrieved 2012-07-17.
- ↑ "GAP-software, decompression simulation software". Gap-software.com. 2008-02-10. Retrieved 2012-07-17.
- ↑ Ultimate Planner – decompression planning software tool http://www.techdivingmag.com/ultimateplanner.html
- ↑ Lang, M.A.; Hamilton, Jr R.W. (1989). Proceedings of the AAUS Dive Computer Workshop. United States: USC Catalina Marine Science Center. p. 231. Retrieved 2008-08-07.
- 1 2 Møllerløkken, Andreas (24 August 2011). S. Lesley Blogg, Michael A. Lang and Andreas Møllerløkken, eds. "Proceedings of Validation of Dive Computers Workshop". Gdansk, Poland: European Underwater and Baromedical Society. Retrieved 3 March 2016.
- 1 2 3 4 Boan, Charlotte (2014). "How to deploy a shotline". Dive magazine archive. Syon publishing. Retrieved 3 March 2016.
- ↑ "Technical Issues". Newry & Mourne Sub Aqua Club. Retrieved 2009-08-28.
- ↑ Staff (2005–2016). "Surface Marker Buoys (SMBs)". Scuba Doctor website. Melbourne: The Scuba Doctor Australia. Retrieved 7 March 2016.
- 1 2 Staff. "Recommendations Concerning the Use of Surface Marker Buoys" (PDF). British Diving Safety Group. Retrieved 7 March 2016.
- ↑ Staff (2015). "Delayed surface marker buoy". BSAC Safe Diving. British Sub-Aqua Club. p. 18. Retrieved 7 March 2016.
- ↑ Nawrocky, Pete (2014). "We're Over Here!". Alert Diver online, Spring 2014. Divers Alert Network. Retrieved 7 March 2016.
- ↑ Staff. "Diving Launch And Recovery Systems". Commercial Diving Equipment. Submarine Manufacturing & Products Ltd. Retrieved 7 March 2016.
- ↑ Staff. "Pommec 2 diver launch and recovery system with diving basket" (PDF). Technical Diving Equipment. Pommec BV. Retrieved 7 March 2016.
- 1 2 Jablonski, Jarrod (2006). "Details of DIR Equipment Configuration". Doing it Right: The Fundamentals of Better Diving. High Springs, Florida: Global Underwater Explorers. p. 113. ISBN 0-9713267-0-3.
- 1 2 Beyerstein, G (2006). Lang, MA; Smith, NE, eds. Commercial Diving: Surface-Mixed Gas, Sur-D-O2, Bell Bounce, Saturation. Proceedings of Advanced Scientific Diving Workshop. Smithsonian Institution, Washington, DC. Retrieved 12 April 2010.
- ↑ Bevan, J. (1999). "Diving bells through the centuries". South Pacific Underwater Medicine Society Journal. 29 (1). ISSN 0813-1988. OCLC 16986801. Retrieved 2008-04-25.
- ↑ Staff (May 2013). "Guidance on Hyperbaric Evacuation Systems" (PDF). Guidance on Hyperbaric Evacuation Systems IMCA D 052 May 2013. International Marine Contractors' Association. Retrieved 6 March 2016.
- ↑ Staff, IDSA,(2009), International Diver Training Certification: Diver Training Standards, Revision 4, October 2009 http://www.idsaworldwide.org/docs/diverts0909.pdf Accessed 13 September 2013
- ↑ Staff (2002). Paul Williams, ed. The Diving Supervisor’s Manual (IMCA D 022 May 2000, incorporating the May 2002 erratum ed.). Carlyle House, 235 Vauxhall Bridge Road, London SW1V 1EJ, UK: International Marine Contractors' Association. ISBN 1-903513-00-6.
- ↑ Staff (2006). "Minimum Course Content for Enriched Air Nitrox Scuba Certification" (PDF). Dive Standards & Medical Statement. Recreational Scuba Training Council (RSTC). Retrieved 15 March 2016.
- ↑ Staff (2004). "Minimum Course Content for Open Water Scuba Certification" (PDF). Dive Standards & Medical Statement. Recreational Scuba Training Council (RSTC). Retrieved 15 March 2016.
- ↑ Staff (June 2012). "Syllabus 3.A.7: CMAS Three Stars Diver Training Programme". CMAS International Diver Training Standards and Procedures Manual. World Confederation of Underwater Activities (C.M.A.S.). Retrieved 14 March 2016.
- ↑ Staff. "BSAC Advanced Diver - Course Overview" (PDF). BSAC Advanced Diver Course Outline. British Sub-Aqua Club. Retrieved 14 March 2016.
- ↑ Committee SF/17 (1992). "2.2.7 Apply decompression tables, and 2.2.8 Use surface decompression". Australian Standard AS2815.3 Training and certification of occupational divers. Part 3: Air diving to 50 m. Homebush NSW.: Standards Association of Australia. pp. 13 –14. ISBN 0726276316.
- ↑ Diving Advisory Board (2003). "1.8 Decompression theory and tables". Class III diver training standard. Pretoria: South African Department of Labour.
Sources
- Ball, R; Himm, J; Homer, LD; Thalmann, ED (1995). "Does the time course of bubble evolution explain decompression sickness risk?". Undersea and Hyperbaric Medicine. 22 (3): 263–280. ISSN 1066-2936. PMID 7580767.
- Brubakk, A. O.; Neuman, T. S. (2003). Bennett and Elliott's physiology and medicine of diving (5th Revised ed.). United States: Saunders. ISBN 0-7020-2571-2.
- Gerth, Wayne A; Doolette, David J. (2007). "VVal-18 and VVal-18M Thalmann Algorithm – Air Decompression Tables and Procedures". Navy Experimental Diving Unit, TA 01-07, NEDU TR 07-09. Retrieved 2012-01-27.
- Hamilton, Robert W; Thalmann, Edward D (2003). "10.2: Decompression Practice". In Brubakk, Alf O; Neuman, Tom S. Bennett and Elliott's physiology and medicine of diving (5th Revised ed.). United States: Saunders. pp. 455–500. ISBN 0-7020-2571-2. OCLC 51607923.
- Huggins, Karl E. (1992). "Dynamics of decompression workshop". Course taught at the University of Michigan. Retrieved 2012-01-10.
- Lippmann, John (1990). Deeper into Diving (1st ed.). Melbourne, Australia: J L Publications. ISBN 0-9590306-3-8.
- Parker, E. C.; S.S. Survanshi, P.K. Weathersby, and E.D. Thalmann. (1992). "Statistically Based Decompression Tables VIII: Linear Exponential Kinetics". Naval Medical Research Institute Report. 92-73. Retrieved 2008-03-16.
- Powell, Mark (2008). Deco for Divers. Southend-on-Sea: Aquapress. ISBN 1-905492-07-3.
- Thalmann, E. D. (1984). "Phase II testing of decompression algorithms for use in the U.S. Navy underwater decompression computer". Navy Exp. Diving Unit Res. Report. 1–84. Retrieved 2008-03-16.
- Thalmann, E. D. (1985). "Development of a Decompression Algorithm for Constant Oxygen Partial Pressure in Helium Diving". Navy Exp. Diving Unit Res. Report. 1–85. Retrieved 2008-03-16.
- US Navy (2008). US Navy Diving Manual, 6th revision. United States: US Naval Sea Systems Command. Retrieved 2008-06-15.
- Wienke, Bruce R; O'Leary, Timothy R (13 February 2002). "Reduced gradient bubble model: Diving algorithm, basis and comparisons" (PDF). Tampa, Florida: NAUI Technical Diving Operations. Retrieved 25 January 2012.
- Yount, DE (1991). "Gelatin, bubbles, and the bends". International Pacifica Scientific Diving... Hans-Jurgen, K; Harper Jr, DE (eds.), (Proceedings of the American Academy of Underwater Sciences Eleventh Annual Scientific Diving Symposium held 25–30 September 1991. University of Hawaii, Honolulu, Hawaii). Retrieved 2012-01-25.
Further reading
- Powell, Mark (2008). Deco for Divers. Southend-on-Sea: Aquapress. ISBN 1-905492-07-3.
- Lippmann, John; Mitchell, Simon (2005). Deeper into Diving (2nd ed.). Melbourne, Australia: J L Publications. ISBN 0-9752290-1-X. Section 2 chapters 13–24 pages 181–350
External links
- Dive tables from the NOAA
- German BGV C 23 table, permitting a simplified procedure of decompression planning
- Online dive table calculator
