Hypertensive kidney disease
| Hypertensive kidney disease | |
|---|---|
| Synonyms | hypertensive nephrosclerosis, hypertensive kidney disease, hypertensive nephropathy |
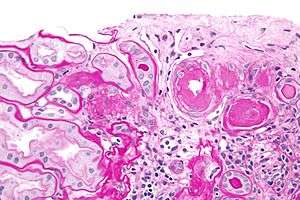 | |
| Micrograph showing renal arterial hyalinosis – pink ring right-of-centre. PAS stain. | |
| Classification and external resources | |
| Specialty | nephrology |
| ICD-10 | I12 |
| ICD-9-CM | 403 |
Hypertensive kidney disease is a medical condition referring to damage to the kidney due to chronic high blood pressure. HN can be divided into two types: benign and malignant. Benign nephrosclerosis is common in individuals over the age of 60 where malignant nephrosclerosis is uncommon and affects 1-5% of individuals with high blood pressure, that have diastolic blood pressure passing 130 mm Hg.[1] It should be distinguished from renovascular hypertension, which is a form of secondary hypertension. In addition, HN can be referred to as hypertensive nephrosclerosis, benign nephrosclerosis, and nephroangiosclerosis.[2]
Signs and symptoms
Symptoms of chronic kidney disease, including loss of appetite, nausea, vomiting, itching, sleepiness or confusion, weight loss, and an unpleasant taste in the mouth, may develop.[3]
Causes
"Hypertensive" refers to high blood pressure and "nephropathy" means damage to the kidney; hence this condition is where chronic high blood pressure causes damages to renal tissue; this includes the small blood vessels, glomeruli, renal tubules and interstitial tissues. The tissue hardens and thickens which is know as nephrosclerosis.[4] The narrowing of the blood vessels means less blood is going to the tissue and so less oxygen is reaching the tissue resulting in tissue death (ischemia).[5]
Risk factors for HN include:
- poorly controlled moderate to high blood pressure
- older age
- other kidney disorders
- Afro-Caribbean background – unclear whether this is due to them being more genetically susceptible to kidney damage by hypertension or whether it is because of poor management of high blood pressure amongst them.[4]
Mechanism
In the kidneys, as a result of benign arterial hypertension, hyaline (pink, amorphous, homogeneous material) accumulates in the wall of small arteries and arterioles, producing the thickening of their walls and the narrowing of the lumina — arteriolosclerosis. Consequent ischemia will produce tubular atrophy, interstitial fibrosis, glomerular alterations (smaller glomeruli with different degrees of hyalinization – from mild to sclerosis of glomeruli) and periglomerular fibrosis. In advanced stages, kidney failure will occur. Functional nephrons[6] have dilated tubules, often with hyaline casts in the lumens. Additional complications often associated with hypertensive nephropathy include glomerular damage resulting in protein and blood in the urine.
Hypertensive nephropathy refers to patients with renal failure that can be attributed to a history of hypertension[7] It is a chronic condition and it is a serious risk factor for the development of end-stage renal disease (ESRD). However, despite the well-known association between hypertension and chronic kidney disease, the underlying mechanism remains unclear. The two proposed mechanisms of HN’s pathophysiology[8] both centre around how the glomerulus, a network of dense capillaries that carries out the kidney filtration process, is affected; with one theory identifying glomerular ischemia as the main contributor to HN and the other identifying glomerular hypertension and glomerular hyperfiltration at the centre of HN’s pathogenesis.
Glomerular ischemia
High blood pressure in the long term can damage the endothelium, commonly known as the blood vessel lining. This leads to a build-up of plaques and they can be deposited in the renal arteries causing stenosis and ischemic renal disease. In this situation, the stenotic kidney suffers from ischemia due to the reduction in blood flow, which in turn causes the size of the kidneys to decrease. Other consequences include arterial stiffening, which involves a gradual breakdown of elastic fibers and intima (the innermost layer of a blood vessel) thickening.
Glomerular hypertension and glomerular hyperfiltration
An alternative mechanism of hypertensive nephropathy is prolonged glomerular hypertension and hence glomerular hyperfiltration. These can occur simultaneously but not necessarily. The idea is that hypertension results in sclerosis of the glomeruli which ultimately means reduced renal function. As a compensatory mechanism, the unaffected nephrons (specifically, the pre-glomerular arterioles) vasodilate to increase renal perfusion (blood flow) and glomerular filtration.
Diagnosis
Diagnosis of HN is made from a clinical history and biochemical investigations. Chronic hypertension with progressively renal insufficiency over a long period of time. Damage to the glomerulus allows proteins that are usually too large to pass into the nephron to be filtered. This leads to an elevated concentration of albumin in the urine. This albuminuria is usually asymptomatic, but can be indicative of numerous kidney disorders. Proteinuria is best identified from a 24-hour urine collection.[9]
Bilateral renal artery stenosis should always be considered as a differential diagnosis for the presentation of HN. Renal disease with this etiology can potentially be reversed following vascular intervention.
Histology
In benign nephrosclerosis, the changes occurring are gradual and progressive, however, there can be sufficient renal reserve capacity to maintain adequate renal function for many years.[10] The large renal arteries exhibit intimal thickening, medial hypertrophy, duplication of the elastic layer. The changes in small arterioles include hyaline arteriolosclerosis (deposition of hyaline, collagenous material),[1] which causes glomerular collapse (wrinkling and thickening of capillary basement membranes and collapse of capillary lumen) and solidification (glomeruli exhibit sclerosis and increase in mesangial matrix). The degree of scarring correlates with the degree of glomerular filtration deficit.
Malignant nephrosclerosis occurs in presence of malignant hypertension (when DBP > 130mmHg). Vessels feature intimal thickening, fibrinoid necrosis, red blood cell fragmentation, extravasation, thrombosis. These changes create an exaggerated layered appearance (onion skinning).[11]
Urine test
Microalbuminuria (moderate increase in the levels of urinary albumin) is a non-specific finding in patients with vascular disease that is associated with increased risk of cardiovascular events. The majority of patients with benign nephrosclerosis have proteinuria in the range from 0.5 to 1 g/ 24hr. In the case of glomerular damage occurring in HN, hematuria can occur as well.[1]
Definitive diagnosis
The definitive diagnosis of HN requires morphological examination. Common histological features can be identified in the renal and glomerular vasculature. Glomerulosclerosis is often present, either focally or globally, which is characterized by hardening of the vessel walls. Also, luminal narrowing or the arteries and arterioles of the renal system. However, this type of procedure is likely to be preceded with a provisional diagnosis based on laboratory investigations.
Future diagnostic approaches
Increasing access to, and use of, genome profiling may provide opportunity for diagnosis based on presentation and genetic risk factors, by identifying ApoL1 gene variants on chromosome 22.[12]
Management
The aim of the medical treatment is to slow the progression of chronic kidney disease by reducing blood pressure and albumin levels.[13] The current published guidelines define ideal BP of <130/80 mmHg for patients with hypertensive nephropathy; studies show that anything higher or lower than this can increase cardiovascular risk. According to the African American Study of Kidney Disease (AASK) trial, after an additional 5 years follow-up upon completion of the 10-year trial, up to 65% of the cohort had progressive nephropathy despite having controlled the mean systolic BP level <135 mmHg.[14]
ACE inhibitors, angiotensin receptor blockers, direct renin inhibitors and aldosterone antagonists, are pharmacological treatments that can be used to lower BP to target levels; hence reducing neuropathy and proteinuria progression. The management plan should be individualized based on the condition of the patients including comorbidities and previous medical history.
In addition, there are lifestyle changes that can be made. Weight reduction, exercise, reducing salt intake can be done to manage hypertensive nephropathy.
Prognosis
According to the United States Renal Data System (USRDS), hypertensive nephropathy accounts for more than one-third of patients on hemodialysis and the annual mortality rate for patients on hemodialysis is 23.3%. Haemodialysis is recommended for patients who progress to end-stage renal disease (ESRD) and hypertensive nephropathy is the second most common cause of ESRD after diabetes. Patient prognosis is dependent on numerous factors including age, ethnicity, blood pressure and glomerular filtration rate. Changes in lifestyle factors, such as reduction in salt intake and increased physical activity have been shown to improve outcomes but are insufficient without pharmacological treatment.
Epidemiology
The incidence of hypertensive nephropathy varies around the world. For instance, it accounts for as many as 25% and 17% of patients starting dialysis for end-stage kidney disease in Italy and France respectively. Contrastingly, Japan and China report only 6 and 7% respectively. Since the year 2000, nephropathy caused by hypertension has increased in incidence by 8.7% [15] In reality, these figures may be even higher, as hypertension is not always reported as the specific cause of kidney disease.[16]
It has been recognized that the incidence of hypertensive nephropathy varies with ethnicity. Compared to Caucasians, African Americans in the USA are much more likely to develop hypertensive nephropathy.[17] Of those who do, the proportion who then go on to develop end-stage renal failure is 3.5 times higher than in the Caucasian population. In addition to this, African Americans tend to develop hypertensive nephropathy at a younger age than Caucasians (45 to 65, compared to >65).[18]
See also
References
- 1 2 3 Tahir, Khawaja; Mujeeb, Muzna; Khalid, Sadia (2010). "Management of Hypertensive nephropathy" (PDF). J Biomed Sci and Res. 2 (4): 295–301.
- ↑ Fervenza, Fernando C (2016-09-08). Batuman, Vecihi, ed. "Nephrosclerosis: Background, Pathophysiology, Epidemiology".
- ↑ "Benign Hypertensive Arteriolar Nephrosclerosis". MSD Manual Consumer Version. Retrieved 2016-11-12.
- 1 2 Zhang, Zhiwei. "Benign Hypertensive Arteriolar Nephrosclerosis". Merck Manuals Consumer Version. Retrieved 2016-11-12.
- ↑ "Hypertensive Nephropathy,Symptoms, Treatment,Diet and Causes – Kidney Disease Symptoms and Treatment". www.kidney-symptom.com. Retrieved 2016-11-12.
- ↑ "nephron: definition of nephron in Oxford dictionary (American English) (US)". www.oxforddictionaries.com. Retrieved 2016-04-15.
- ↑ "Nephrosclerosis: Background, Pathophysiology, Epidemiology". 2016-09-08.
- ↑ Suneel Udani, MD; Ivana Lazich, MD; George L. Bakris, MD. "Epidemiology of Hypertensive Kidney Disease".
- ↑ Rowe, D J; Bagga, H; Betts, P B (1985-09-14). "Normal variations in rate of albumin excretion and albumin to creatinine ratios in overnight and daytime urine collections in non-diabetic children". British Medical Journal (Clinical research ed.). 291 (6497): 693–694. ISSN 0267-0623. PMC 1416648
 . PMID 3929903.
. PMID 3929903. - ↑ MD, Edward C. Klatt. "Renal Pathology". library.med.utah.edu. Retrieved 2016-11-12.
- ↑ http://library.med.utah.edu/WebPath/RENAHTML/RENAL107.html
- ↑ Parsa, Afshin; Kao, W. H. Linda; Xie, Dawei; Astor, Brad C.; Li, Man; Hsu, Chi-yuan; Feldman, Harold I.; Parekh, Rulan S.; Kusek, John W. (2013-12-05). "APOL1 risk variants, race, and progression of chronic kidney disease". The New England Journal of Medicine. 369 (23): 2183–2196. doi:10.1056/NEJMoa1310345. ISSN 1533-4406. PMC 3969022
 . PMID 24206458.
. PMID 24206458. - ↑ "Clinical features, diagnosis, and treatment of hypertensive nephrosclerosis". www.uptodate.com. Retrieved 2016-11-12.
- ↑ Hart, Peter D.; Bakris, George L. (2010-11-01). "Hypertensive nephropathy: prevention and treatment recommendations". Expert Opinion on Pharmacotherapy. 11 (16): 2675–2686. doi:10.1517/14656566.2010.485612. ISSN 1744-7666. PMID 20718588.
- ↑ Fervenza, Fernando (2015-03-30). "Nephrosclerosis". Medscape. Retrieved 2016-11-12.
- ↑ Yarnell, John; O'Reilly, Dermot (2013-05-23). Epidemiology and Disease Prevention: A Global Approach. OUP Oxford. ISBN 978-0-19-966053-7.
- ↑ Fogo, Agnes B. (2003-02-01). "Hypertensive risk factors in kidney disease in African Americans". Kidney International. Renal Disease in Racial and Ethnic Minority Groups. 63, Supplement 83: S17–S21. doi:10.1046/j.1523-1755.63.s83.5.x.
- ↑ "Nephrosclerosis: Background, Pathophysiology, Epidemiology". 2016-09-08.
External links
- Photo at Atlas of Pathology
- Tylicki L, Rutkowski B (2003). "Hypertensive nephropathy: pathogenesis, diagnosis and treatment". Pol. Merkur. Lekarski (in Polish). 14 (80): 168–73. PMID 12728683.
- Luft FC (October 2000). "Hypertensive nephrosclerosis-a cause of end-stage renal disease?". Nephrol Dial Transplant. 15 (10): 1515–7. doi:10.1093/ndt/15.10.1515. PMID 11007815.