Danazol
 | |
| Clinical data | |
|---|---|
| Trade names | Azol, Bonzol, Cyclomen, Danol, Nazol |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682599 |
| Pregnancy category | |
| Routes of administration | Oral |
| ATC code | G03XA01 (WHO) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Metabolism | Hepatic[1] |
| Biological half-life | 3–6 hours (acute), 24–26 hours (chronic)[1] |
| Excretion | Urine, feces[1] |
| Identifiers | |
| |
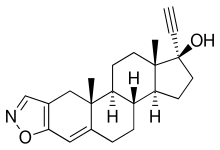
| Synonyms | WIN-17757; 17α-ethinyl-17β-hydroxy-4-androsten-[2,3-d]isoxazole |
| CAS Number |
17230-88-5 |
| PubChem (CID) | 28417 |
| IUPHAR/BPS | 6942 |
| DrugBank |
DB01406 |
| ChemSpider |
26436 |
| UNII |
N29QWW3BUO |
| KEGG |
D00289 |
| ChEBI |
CHEBI:4315 |
| ChEMBL |
CHEMBL1479 |
| Chemical and physical data | |
| Formula | C22H27NO2 |
| Molar mass | 337.5 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
| (verify) | |
Danazol (INN, USAN, BAN, JAN) (brand names Danocrine, Danol, Danazol, Danatrol, Danoval, Cyclomen, many others), also known as 17α-ethinyl-17β-hydroxy-4-androsten-[2,3-d]isoxazole, is a synthetic steroid that is used primarily in the treatment of endometriosis and is marketed widely throughout the world.[1][2][3][4] It is the derivative of ethisterone (17α-ethynyltestosterone) where the 3-ketone is replaced with a 2,3-isoxazole moiety.[5][6] Danazol was approved by the US Food and Drug Administration as the first drug to specifically treat endometriosis in 1971.[5][7] Although effective for endometriosis, its use is limited by its masculinizing side effects.[8] Since their introduction, danazol has largely been replaced by gonadotropin-releasing hormone (GnRH) agonists in the treatment of the condition.[9]
Indications
Danazol has been used—mostly off-label—for other indications, namely in the management of menorrhagia, fibrocystic breast disease, immune thrombocytopenic purpura, premenstrual syndrome, breast pain, and hereditary angioedema.[10] Although not currently a standard treatment for menorrhagia, danazol demonstrated significant relief in young women with menorrhagia in a study, and, because of a lack of a significant adverse effects, it was proposed as an alternative treatment.[11] Low-dose danazol has also been investigated in the treatment of diabetic macular edema in a phase III clinical trial.[12][13] A dosage of 800 mg/day danazol was found to increase telomere length in patients with telomere diseases in a phase I/II clinical trial.[14]
Side effects
Androgenic side effects are of concern, as some women taking danazol may experience unwanted hair growth (hirsutism), acne, irreversible deepening of the voice,[9] or adverse blood lipid profiles.[15] In addition, breast atrophy and decreased breast size may occur.[9] The drug may also cause hot flashes, elevation of liver enzymes, and mood changes.[15] Some patients who use danazol experience weight gain and fluid retention. Due to its side effects, danazol is seldom prescribed continuously beyond six months.
The use of danazol for endometriosis has been linked to an increased risk of ovarian cancer.[16] Patients with endometriosis have specific risk factors for ovarian cancer, so this may not apply for other uses.
Danazol, like most other androgenic drugs, has been linked with an increased risk of liver tumors. These are generally benign.[17]
Contraindications
Danazol is contraindicated during pregnancy because it has the potential to virilize female fetuses. Women taking danazol should practice effective contraception to prevent pregnancy if sexually active.[15]
Since danazol is metabolized by the liver, it cannot be used by patients with liver disease, and in patients receiving long-term therapy, liver function must be monitored on a periodic basis.
Pharmacology
Danazol possesses a complex pharmacology, with multiple mechanisms of action.[5][18][19] These include direct binding to and activation of sex hormone receptors, direct inhibition of enzymes involved in steroidogenesis, and direct binding to and occupation of steroid hormone carrier proteins and consequent displacement of steroid hormones from these proteins.[5][9][18][19] The drug is characterized as a weak androgen and anabolic, a weak progestogen, a weak antigonadotropin, and a functional antiestrogen.[5][20]
Modulation of steroid hormone receptors
The steroid hormone receptor activity profile of danazol is as follows:[9][18]
| Receptor | Affinity | Effect |
|---|---|---|
| Androgen receptor | 90 nM | Agonist |
| Progesterone receptor | 6,000 nM | Agonist-antagonist |
| Glucocorticoid receptor | 5,000 nM | Agonist |
| Estrogen receptor | 80,000 nM | Agonist |
As such, danazol is described as a possessing high affinity for the AR, moderate affinity for the PR and GR, and poor affinity for the ER.[18] As an androgen, danazol is described as weak, being about 200-fold less potent than testosterone in bioassays.[20] The drug can act as both an agonist and antagonist of the PR depending on the bioassay, indicating that it could be regarded as a selective progesterone receptor modulator.[18] Although the affinity and efficacy of danazol itself at the PR are relatively low, ethisterone, one of the major metabolites of danazol, is described as a weak progestogen (and has been employed clinically as a progestogenic contraceptive), and this presumably balances the in vivo progestogenic activity of danazol.[21] The activity of danazol at the ER is considered to be minimal, although at very high concentrations the drug can act significantly as an ER agonist.[18] Danazol is considered to act significantly as an agonist of the GR, and thus, as a glucocorticoid.[18] In accordance, it can suppress the immune system.[5][18][20]
Inhibition of steroidogenesis enzymes
Danazol has been found to act as an inhibitor of the following steroidogenesis enzymes:[18]
| Enzyme | Affinity (Ki) | Inhibition type | Est. inhibition at 2 μM |
|---|---|---|---|
| Cholesterol side-chain cleavage enzyme | 20 μM | Competitive | ? |
| 3β-Hydroxysteroid dehydrogenase/Δ5-4 isomerase | 5.8 μM | Competitive | 4.3% |
| 17α-Hydroxylase | 2.4 μM | Competitive | 2.9% |
| 17,20-Lyase | 1.9 μM | Competitive | 3.9% |
| 17β-Hydroxysteroid dehydrogenase | 4.4 μM | Competitive | 15% |
| 21-Hydroxylase | 0.8 μM | Competitive | 37% |
| 11β-Hydroxylase | 1 μM | Competitive | 21% |
| Aromatase | >100 μM | – | 0% |
Danazol has also been found to be a weak inhibitor of steroid sulfatase (Ki = 2.3–8.2 μM), the enzyme that converts DHEA-S to DHEA and estrone sulfate to estrone (which can then subsequently be transformed into estrone (with androstenedione as an intermediate) and estradiol, respectively).[22] Although in contradiction with the above data, another study found that danazol weakly inhibited aromatase as well, with 44% inhibition at a concentration of 10 μM.[22]
For reference, circulating concentrations of danazol are in the range of 2 μM at a dosage of 600 mg/day in women.[18]
In accordance with the above, clinical studies have demonstrated that danazol directly and markedly inhibits adrenal, ovarian, and testicular steroidogenesis in vivo.[18] The enzymatic production of estradiol, progesterone, and testosterone have all specifically been found to be inhibited.[18]
Occupation and downregulation of carrier proteins
Danazol is known to bind to two steroid hormone carrier proteins: sex hormone-binding globulin (SHBG), which binds androgens and estrogens; and transcortin (corticosteroid-binding globulin), which binds progesterone and cortisol.[9][18] Binding of danazol to SHBG is considered to be more important clinically.[18] By occupying SHBG and transcortin, danazol increases the ratio of free to plasma protein-bound testosterone, estradiol, progesterone, and cortisol.[9][18] The following table shows the difference in testosterone levels in untreated premenopausal women and women treated with danazol:[18]
| Group | Free | Albumin | SHBG |
|---|---|---|---|
| Normal (no danazol) | 1% | 39% | 60% |
| Danazol treatment | 3% | 79% | 18% |
As can be seen, the percentage of free testosterone is tripled in women being treated with danazol.[18][23] The ability of danazol to increase free testosterone levels suggests that a portion of its weak androgenic effects are mediated indirectly by facilitating the activity of testosterone and dihydrotestosterone through the displacement of them from SHBG.[18][23] In addition to binding to and occupying SHBG however, danazol also decreases the hepatic production of SHBG and therefore SHBG levels, and so downregulation of SHBG may be involved as well.[9][18] Danazol likely decreases hepatic production of SHBG by reducing estrogenic and increasing androgenic activity in the liver (as androgens and estrogens increase and decrease, respectively, hepatic SHBG synthesis).[24] In accordance with the notion that suppression of SHBG is involved in the androgenic effects of danazol, the drug has synergistic rather than additive androgenic effects in combination with testosterone in bioassays (which is most likely secondary to the increased free testosterone levels).[20]
It is noteworthy that 2-hydroxymethylethisterone, a major metabolite of danazol, circulates at concentrations 5–10 times greater than those of danazol and is twice as potent as danazol in displacing testosterone from SHBG.[25] As such, most of the occupation of SHBG by danazol may actually be due to this metabolite.[25]
Antigonadotropic activity
Via its weak progestogenic and androgenic activity, through activation of the PR and AR in the pituitary gland, danazol produces antigonadotropic effects.[18] Although its does not significantly affect basal luteinizing hormone (LH) and follicle-stimulating hormone (FSH) levels in premenopausal women (and hence does not profoundly suppress gonadotropin or sex hormone levels like other, stronger antigonadotropins do),[26] the drug prevents the mid-cycle surge in the levels of these hormones during the menstrual cycle.[9][15][20][27][28] By doing this, it suppresses increases in estrogen and progesterone levels at this time and prevents ovulation.[15][20][27][28]
Mechanism of action in endometriosis
Because danazol reduces estrogen production and levels,[26] it has functional antiestrogenic properties.[29] The combination of its antiestrogenic, androgenic, and progestogenic or antiprogestogenic actions cause atrophy of the endometrium, which alleviates the symptoms of endometriosis.[9][18][20][26][30]
Pharmacokinetics
Danazol has an elimination half-life of 3–6 hours after a single dose and 24–26 hours with repeated administration.[1] Its major metabolites are 2-hydroxymethylethisterone (formed by CYP3A4 and described as inactive) and ethisterone,[6][31][32] and other, minor metabolites include ∆2-hydroxymethylethisterone, 6β-hydroxy-2-hydroxymethylethisterone, and ∆1-6β-hydroxy-2-hydroxymethylethisterone.
History
Danazol was synthesized in 1963 by a team of scientists at Sterling Winthrop in Rensselaer, New York by a team that included Helmutt Neumann, Gordon Potts, W.T. Ryan, and Frederik W. Stonner.[33][34]
Clinical trial
A 2016 phase 1–2 prospective study orally administered 800 mg per day to 27 patients with telomere diseases. The primary efficacy endpoint was a 20% reduction in the annual rate of telomere attrition measured. Toxic effects formed the primary safety endpoint. The study was halted early, after telomere attrition was reduced in all 12 patients who could be evaluated. 12 of 27 patients achieved the primary efficacy end point, 11 of whom increased telomere length at 24 months. Hematologic responses (secondary efficacy endpoint) occurred in 10 of 12 patients who could be evaluated at 24 months. Elevated liver-enzyme levels and muscle cramps (known adverse effects) of grade 2 or less occurred in 41% and 33% of the patients, respectively.[35]
See also
References
- 1 2 3 4 5 Brayfield, A, ed. (30 October 2013). "Danazol". Martindale: The Complete Drug Reference. Pharmaceutical Press. Retrieved 1 April 2014.
- ↑ J. Elks (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 345–. ISBN 978-1-4757-2085-3.
- ↑ Index Nominum 2000: International Drug Directory. Taylor & Francis. January 2000. pp. 293–. ISBN 978-3-88763-075-1.
- ↑ I.K. Morton; Judith M. Hall (6 December 2012). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Science & Business Media. pp. 91–. ISBN 978-94-011-4439-1.
- 1 2 3 4 5 6 Howard W. Jones; John A. Rock (10 July 2015). Te Linde's Operative Gynecology. Wolters Kluwer Health. pp. 1327–1330. ISBN 978-1-4963-1521-2.
- 1 2 Thomas L. Lemke; David A. Williams (24 January 2012). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. pp. 1361–. ISBN 978-1-60913-345-0.
- ↑ Dmowski WP, Scholer HF, Mahesh VB, Greenblatt RB (1971). "Danazol--a synthetic steroid derivative with interesting physiologic properties". Fertil. Steril. 22 (1): 9–18. PMID 5538758.
- ↑ Selak V, Farquhar C, Prentice A, Singla A (2007). Farquhar, Cindy, ed. "Danazol for pelvic pain associated with endometriosis". Cochrane database of systematic reviews (Online) (4): CD000068. doi:10.1002/14651858.CD000068.pub2. PMID 17943735.
- 1 2 3 4 5 6 7 8 9 10 Eberhard Nieschlag; Hermann M. Behre; Susan Nieschlag (13 January 2010). Andrology: Male Reproductive Health and Dysfunction. Springer Science & Business Media. pp. 426–428. ISBN 978-3-540-78355-8.
- ↑ Rod Flower; Humphrey P. Rang; Maureen M. Dale; Ritter, James M. (2007). Rang & Dale's pharmacology. Edinburgh: Churchill Livingstone. ISBN 0-443-06911-5.
- ↑ "Efficacy of vaginal danazol treatment in women with menorrhagia during fertile age". Fertil. Steril. 92 (4): 1351–4. October 2009. doi:10.1016/j.fertnstert.2008.08.017. PMID 18930222.
- ↑ "A Safety and Efficacy Study of Oral Danazol (a Previously Approved Drug)in the Treatment of Diabetic Macular Edema". Clinicaltrials.gov. Ampio Pharmaceuticals. Inc. Retrieved 27 June 2015.
- ↑ "Ampio Pharmaceuticals Announces Additional Statistically Significant Study Results for Optina™ in the Treatment of Diabetic Macular Edema (DME)". Ampio Pharmaceuticals. Inc. Retrieved 27 June 2015.
- ↑ "Danazol Treatment for Telomere Diseases". N.E.J.M. 374 (20): 1922–31. May 2016. doi:10.1056/NEJMoa1515319.
- 1 2 3 4 5 Hoffman, Barbara L; Schorge JO; Schaffer JI; Halvorson LM; Bradshaw KD; Cunningham FG; Calver LE. Williams Gynecology: Chapter 10, Endometriosis (2nd ed.). New York: McGraw-Hill Medical. ISBN 9780071716727.
- ↑ Cottreau CM, Ness RB, Modugno F, Allen GO, Goodman MT (2003). "Endometriosis and Its Treatment with Danazol or Lupron in Relation to Ovarian Cancer". Clinical Cancer Research. 9 (14): 5142–4. PMID 14613992.
- ↑ Velazquez I, Alter BP (2004). "Androgens and liver tumors: Fanconi's anemia and non-Fanconi's conditions". Am. J. Hematol. 77 (3): 257–67. doi:10.1002/ajh.20183. PMID 15495253.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 Eric J. Thomas; John Rock (6 December 2012). Modern Approaches to Endometriosis. Springer Science & Business Media. pp. 239–256. ISBN 978-94-011-3864-2.
- 1 2 Aurel Lupulescu (24 October 1990). Hormones and Vitamins in Cancer Treatment. CRC Press. pp. 103–. ISBN 978-0-8493-5973-6.
- 1 2 3 4 5 6 7 Albert Altchek; Liane Deligdisch; Nathan Kase (4 September 2003). Diagnosis and Management of Ovarian Disorders. Academic Press. pp. 376–. ISBN 978-0-08-049451-7.
- ↑ Robert J. Kurman (17 April 2013). Blaustein's Pathology of the Female Genital Tract. Springer Science & Business Media. pp. 390–. ISBN 978-1-4757-3889-6.
- 1 2 Shields-Botella, J.; Chetrite, G.; Meschi, S.; Pasqualini, J.R. (2005). "Effect of nomegestrol acetate on estrogen biosynthesis and transformation in MCF-7 and T47-D breast cancer cells". The Journal of Steroid Biochemistry and Molecular Biology. 93 (1): 1–13. doi:10.1016/j.jsbmb.2004.11.004. ISSN 0960-0760.
- 1 2 Richard A. Helms; David J. Quan (2006). Textbook of Therapeutics: Drug and Disease Management. Lippincott Williams & Wilkins. pp. 383–. ISBN 978-0-7817-5734-8.
- ↑ Sarah H. Wakelin; Howard I. Maibach; Clive B. Archer (21 May 2015). Handbook of Systemic Drug Treatment in Dermatology, Second Edition. CRC Press. pp. 23–. ISBN 978-1-4822-2286-9.
- 1 2 Ulrich Westphal (6 December 2012). Steroid-Protein Interactions II. Springer Science & Business Media. pp. 256–. ISBN 978-3-642-82486-9.
- 1 2 3 C. David Tollison; John R. Satterthwaite; Joseph W. Tollison (January 2002). Practical Pain Management. Lippincott Williams & Wilkins. pp. 479–. ISBN 978-0-7817-3160-7.
- 1 2 Floyd, WS (1980). "Danazol: endocrine and endometrial effects.". Int J Fertil. 25 (1): 75–80. PMID 6104649.
- 1 2 Katzung, Bertram (2012). Basic & Clinical Pharmacology (12 ed.). McGraw Hill. p. 732. ISBN 978-0-07-176401-8.
- ↑ Robert B. Taylor (25 September 1998). Taylor’s Family Medicine Review. Springer New York. p. 221. ISBN 978-0-387-98569-5.
- ↑ Fedele, L; Marchini, M; Bianchi, S; Baglioni, A; Bocciolone, L; Nava, S (July 1990). "Endometrial patterns during danazol and buserelin therapy for endometriosis: comparative structural and ultrastructural study.". Obstetrics and gynecology. 76 (1): 79–84. PMID 2113661.
- ↑ Ashraf Mozayani; Lionel Raymon (18 September 2011). Handbook of Drug Interactions: A Clinical and Forensic Guide. Springer Science & Business Media. pp. 646–. ISBN 978-1-61779-222-9.
- ↑ Florencio Zaragoza Dörwald (4 February 2013). Lead Optimization for Medicinal Chemists: Pharmacokinetic Properties of Functional Groups and Organic Compounds. John Wiley & Sons. pp. 485–. ISBN 978-3-527-64565-7.
- ↑ G.P. Ellis and G.B. Ellis, doi:10.1016/S0079-6468(08)70187-5 (1979), pp. 126, note 158, 130, notes 1513, 2369, citing doi:10.1021/jm00299a034
- ↑ Alan N. Elias; Grant Gwinup (1 January 1983). Hirsutism. Praeger. p. 70.
- ↑ Townsley, Danielle M.; Dumitriu, Bogdan; Liu, Delong; Biancotto, Angélique; Weinstein, Barbara; Chen, Christina; Hardy, Nathan; Mihalek, Andrew D.; Lingala, Shilpa (2016-05-18). "Danazol Treatment for Telomere Diseases". New England Journal of Medicine. 374 (20): 1922–1931. doi:10.1056/nejmoa1515319.